Picture this: It’s 2 a.m. You’re doomscrolling, guiltily munching on stale cookies, half-heartedly promising that tomorrow you’ll finally get your life together. Why do we leap for external solutions when something feels off inside? Harvard psychiatrist Dr. K has a story that might just rewire your brain (figuratively, not literally). Let’s unpack why your instinct to chase new jobs or diets might miss the real problem, and what neuroscience, spirituality, and a healthy dose of self-inquiry suggest instead.
The Myth of Quick Fixes: Why Surface Solutions (Almost) Never Work
It’s a pattern you might recognize in your own life: when you’re unhappy, stressed, or struggling, your first instinct is to find a solution—fast. Maybe you think a better job will fix your dissatisfaction, or that improving your looks will solve your dating woes. This urge to jump straight to external fixes is so common that it almost feels automatic (0:00–0:05). But as Harvard Psychiatry and leading Harvard psychiatrists point out, this approach rarely leads to true, lasting change, especially when it comes to mental health disorders.
Dr. K, a Harvard psychiatrist, calls this approach “toxic fuel.” It’s the idea that you can pour something sweet or positive on top of something fundamentally broken and expect it to work. He uses a vivid analogy: if you have a glass of water and someone contaminates it, adding sugar won’t make it clean again (0:12–0:18). The sweetness doesn’t erase the pollution. In the same way, no amount of external upgrades—more money, new relationships, or fancy distractions—can truly heal deep-seated emotional wounds or mental health disorders.
Let’s break this down further. When you’re facing internal struggles, it’s tempting to believe that changing something outside yourself will be the answer. But research shows that surface solutions often mask the real problem, preventing deeper self-understanding and genuine healing. This is especially relevant in the field of Harvard Psychiatry, where experts emphasize that sustainable behavior change starts from within, not from external circumstances.
Here’s a personal example: after a tough breakup, I convinced myself that buying expensive headphones would somehow cure my heartbreak. It didn’t. The pain was still there, just with better sound quality. This kind of “retail therapy” is a classic example of toxic fuel—trying to patch over emotional pain with material goods or temporary pleasures. It’s a distraction, not a solution.
Harvard psychiatrists and mental health professionals see this pattern all the time. Many patients come in hoping for a quick fix, whether it’s a new medication, a different job, or a change in appearance. But as Dr. K puts it,
“No amount of building something good will remove something bad in order to change behavior…what you need to do is save…”
– Dr. K (0:20–0:27)
This insight is crucial, especially in the context of treatment-resistant mental health disorders. Studies indicate that a significant portion of patients do not respond to standard psychiatric treatments, leading to a crisis in mental health care. Harvard Psychiatry research highlights the need for approaches that go beyond surface-level interventions. Internal alignment—addressing the root causes of distress, not just the symptoms—is the foundation for real, sustainable behavior change.
Jumping to quick fixes can actually prevent you from gaining the self-awareness needed for true healing. It’s like putting a bandage on a wound that needs stitches. The bandage might cover it up for a while, but the underlying issue remains. Harvard psychiatrists stress the importance of blending clinical expertise with lived experience, recognizing that real change happens when you address both the mind and the underlying emotional landscape.
So, the next time you’re tempted by a quick external fix, remember the polluted water analogy. Surface solutions might offer temporary relief, but they rarely lead to lasting transformation. True behavior change—and real progress in overcoming mental health disorders—begins with looking inward, not outward.
The Science & Spirit Tango: Neuroscience Meets Ancient Traditions
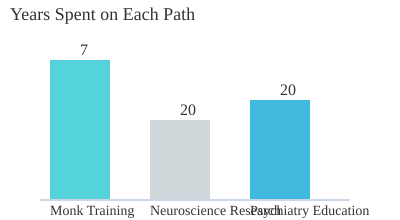
Imagine a life where ancient wisdom and cutting-edge science aren’t at odds, but instead, work together to help you understand yourself. That’s the heart of Dr. K’s journey—a psychiatrist who spent seven years as a monk before training at Harvard Medical School (0.29-0.30). His story is a rare blend of personal struggle, spiritual discipline, and rigorous neuroscience research. It’s a path that shows you don’t have to choose between mindfulness and modern psychiatry; you can use both.
Dr. K’s background is unique. He’s walked the path of a monk, then pivoted to specialize in modern mental health, blending neuroscience with real-life experience (0.30-0.33). This unusual combination gives him a perspective that few psychiatrists have. He’s seen firsthand how meditation and mindfulness can quiet the mind, but he’s also studied the brain’s wiring in clinical settings. Harvard Medical School’s psychiatry research, where Dr. K trained, is at the forefront of exploring how these two worlds intersect.
You might wonder, “Why do I feel lost, anxious, or disconnected—even when I know what’s ‘good’ for me?” Dr. K often says it’s because most people never read the manual for their own mind. We’re not given instructions for handling loneliness, social anxiety, or even falling in love (0.33-0.39). Instead, we’re left to figure things out on our own, often doing the wrong things. For example, talking about your problems can sometimes make things worse if you don’t know how to do it properly (0.43-0.48). And the struggle to fall in love? It’s often tied to dopamine exhaustion from constant device use (0.54-0.56).
This is where neuroscience research and ancient traditions meet. Meditation and mindfulness—practices rooted in centuries-old wisdom—are now backed by neuroscience. Studies at Harvard Medical School and other leading institutions show that these practices can foster self-awareness and emotional balance. The concept of neuroplasticity, for example, reveals that personal change isn’t just a hopeful idea. It’s a biological reality: your brain can rewire itself, given the right tools and habits.
During a silent retreat, Dr. K had an “aha” moment. He realized that both neuroscience and meditation were pointing toward the same truth: the mind’s chaos can be quieted, but you need the right approach. Whether you’re practicing mindfulness or engaging in therapy, the goal is the same—understanding yourself and finding balance.
Harvard psychiatrists are deeply involved in research and education, focusing on how clinical work and neuroscience can address today’s mental health challenges. There’s a growing recognition that mental health disorders are on the rise, and traditional treatments don’t always work for everyone. That’s why integrating mindfulness and neuroscience into clinical work is becoming more common.
“There are two great traditions that have taught us about how humans work—spirituality and science.” – Dr. K
The key insight? Ancient wisdom and modern science don’t have to be rivals. They can be teammates, giving you a more complete “manual” for self-understanding. As you explore the science and spirit tango, you’ll find practical tools—grounded in both mindfulness and psychiatry research—that help unlock your true potential.
Diagnosing the Diagnosis: From TikTok Myths to Medical Reality
If you’ve spent any time on social media lately, you’ve probably noticed a surge in conversations about Mental Health Disorders. Over the past decade, there’s been a revolution in how we talk about mental health—especially on platforms like TikTok (6.27-6.34). This “TikTok-ification” of mental health has brought both positive change and new challenges to the way we understand and approach Diagnosis.
The Good: Awareness and Acceptance
Let’s start with the upside. Thanks to the internet, more people now recognize that their struggles are real and treatable. Ten years ago, many individuals didn’t realize that what they were experiencing—like difficulty getting out of bed or feeling unmotivated—could be symptoms of depression or another mental illness (6.47-7.17). Instead, they blamed themselves, thinking they lacked willpower or discipline. Now, there’s a growing recognition that Mental Health Disorders are not personal failings but medical conditions with real solutions. This shift has had a significant Mental Illness Impact on how people seek help and talk about their experiences.
The Bad: The Rise of Self-Diagnosis
But there’s a flip side. As Dr. K points out, “The biggest problem is that everyone is jumping to a conclusion on the internet which then causes problems because that may not be the right conclusion” (8.36-8.43). With a few swipes, anyone can become a self-taught psychiatrist. Short videos claim that if you forget your keys, you must have ADHD, or if your child throws a tantrum, they’re bipolar (7.54-8.13). This oversimplification skips the most crucial part of Psychiatry Education: differential diagnosis.
Why Differential Diagnosis Matters
Here’s where things get tricky. Losing your keys, for example, could mean you’re distracted, tired, or just having a rough morning. But it could also signal depression, ADHD, anemia, or even sleep apnea (8.22-8.36). The same symptom can have multiple underlying causes. Physicians spend years learning to tease apart these possibilities, using careful evaluation and clinical reasoning—skills that can’t be replaced by a viral video.
Let’s be honest: even professionals sometimes struggle to pinpoint the exact cause of a symptom. I once convinced myself I had ADHD because I kept forgetting where I put my tea mug. Turns out, I was just distracted by my cat. It’s a reminder that real Diagnosis is nuanced. It’s not about slapping on a label, but about understanding what’s truly going on beneath the surface.
Research and the Global Impact
Research shows that Mental Health Disorders are on the rise globally, contributing to human suffering and economic loss. This makes it even more important to get the diagnosis right. Harvard psychiatrists emphasize that gold-standard mental health care requires rigorous evaluation, not just symptom-matching. Mislabeling can lead to the wrong treatment and missed opportunities for real recovery.
“The biggest problem is that everyone is jumping to a conclusion on the internet which then causes problems because that may not be the right conclusion.” – Dr. K
Symptoms and Their Many Causes
Common Symptoms & Possible Diagnoses
Fatigue
Depression
Anemia
Sleep Apnea
Forgetfulness
ADHD
Depression
Trauma
Low Motivation
Depression
Sleep Apnea
Anemia
As you can see, the same symptom can point to several different Mental Health Disorders or even physical conditions. That’s why expert evaluation matters. The internet can raise awareness, but it can’t replace the careful, nuanced approach of a trained professional.
The Dopamine Dilemma: Devices, Distractions, and the Loneliness Epidemic
You’ve probably noticed it yourself: falling in love feels harder, and everywhere you look, people are talking about the loneliness epidemic and rising social anxiety. According to Dr. K, “Loneliness epidemic, social anxiety is increasing, and falling in love seems harder…” (0.37-0.40). But why is this happening, especially when we’re more digitally connected than ever? The answer, research shows, is rooted in a complex mix of mental health crisis, dopamine depletion, and the way our brains interact with modern technology.
Devices and Dopamine: Why Quick Hits Leave Us Empty
Every time you check your phone, swipe on a dating app, or scroll through social media, your brain gets a tiny hit of dopamine. These quick rewards train your mind to crave more of the same, but there’s a catch: the more you chase these instant pleasures, the less satisfying real-life connections become (0.54-0.58). Dr. K points out that we’re “exhausting our dopamine through things like devices,” and most people don’t even realize it’s happening.
This constant stimulation leads to what experts call dopamine depletion. The brain’s reward system gets overloaded, making genuine, meaningful interactions—like meeting someone new or having a deep conversation—feel less rewarding. It’s no wonder that swiping through dating apps often feels less satisfying than an awkward first date in real life.
Rusty Social Skills in a Hyper-Connected World
Texting and messaging have replaced much of our face-to-face communication. While it might seem like we’re more connected, the reality is that our social skills are getting rusty. The parts of your brain that used to be reassured by in-person interactions are now “starting to rust” because of endless texting (1.01-1.08). This shift is linked to the rise in social anxiety, as people lose confidence in real-world social situations.
Harvard Psychiatry has spotlighted this trend, noting that the loneliness epidemic is not just a buzzword—it’s a genuine public health concern. Studies indicate that mental illnesses like depression and anxiety are now among the leading causes of death and ill health worldwide. The impact is profound, touching not just individuals but entire communities.
Modern Lifestyles and the Mental Health Crisis
It’s not just about devices. Modern lifestyles, with their fast pace and constant distractions, are depleting the neurochemistry that underpins healthy relationships. Research from Harvard’s Department of Global Health and Social Medicine shows that the way we live today is contributing to a global mental health crisis. Social medicine experts emphasize the need to rethink how we approach connection and care, especially as treatment-resistant mental illnesses become more common.
Data Snapshot: The Growing Crisis
| Trend | Observation |
|---|---|
| Spike in Social Anxiety Cases | Significant increase over the last decade |
| Global Loneliness Rates | Marked rise, especially among young adults |
All those texts and digital connections? They might actually be making us worse at real relationships, not better. The challenge now is to recognize the patterns, understand the science, and start making changes that support genuine connection—before the loneliness epidemic becomes even more entrenched.
Men, Women, and the Inside Job: Why Fixing the World Might Start with You
When you think about changing your life, where do you look first? If you’re like many men, your first instinct might be to focus on external achievements—earning more money, gaining status, or hitting new fitness goals. But as Harvard Psychiatry research and real-life stories show, the most important changes often happen on the inside (9.44-9.56).
Society tends to train men to solve problems outwardly. You might hear messages like, “Get a better car,” or “Bench more at the gym.” These are tangible goals, but they don’t address the root of most struggles. In fact, the majority of the work that leads to lasting change is internal—learning to understand and manage your own emotions, thoughts, and reactions (9.54-10.00).
EQ vs IQ: The Data Twist
Here’s a surprising fact from the world of high achievers: the top 1% of earners actually have a lower IQ than the top 10%. What sets them apart isn’t raw intelligence, but emotional intelligence (EQ). As Dr. K explains, “The big difference there is that people in the top 1% have a very high EQ.” (10.14-10.28) This means that being able to understand and control yourself—and relate to others—matters more than just being smart. If you want to reach your full potential, focusing on internal change and EQ is key.
| Group | IQ | EQ |
|---|---|---|
| Top 10% Earners | Higher | Lower |
| Top 1% Earners | Lower | Much Higher |
Transformation from the Inside Out: A Real-Life Example
Consider the story of one of Dr. K’s patients. At 32, this man had been using drugs since he was 13—mostly opiates and heroin. He had no job, no stable home, and was crashing with his girlfriend (10.44-10.59). But within just four years, he transformed his life. He became a therapist, secured a stable income, got married, and even published his first novel. This wasn’t about chasing job titles or external validation. It was about mastering self-understanding and emotional regulation (11.01-11.18).
| Before | After (4 Years) |
|---|---|
| Heroin addiction, unstable life | Therapist, stable career, published author |
Why Men and Women Experience Change Differently
It’s important to note that women often approach mental health differently. Traditional therapy and talk-based tools tend to fit women’s emotional articulation better, sometimes leaving men feeling lost. There’s also a biological component—hormones like estrogen can affect emotional awareness and expression, adding another layer to the puzzle.
Social Medicine and the Bigger Picture
Research shows that mental health is deeply connected to social and biological factors. For example, individuals with obesity are more likely to develop conditions like ADHD and depression. This highlights the importance of social medicine—a field championed by leaders like Paul Farmer, who focused on improving mental health care delivery worldwide. The lessons from Harvard Psychiatry and social medicine remind us that lasting change is both an inside job and a community effort.
What If We Taught EQ Like Résumé Writing?
Imagine if job training programs focused as much on self-reflection and emotional intelligence as they do on technical skills. The results could be transformative—not just for individuals, but for society as a whole.
Harvard Insights, Ancient Wisdom: Learning to Read Your Own Manual
Imagine if you had a manual for your mind—a guide to understanding your thoughts, emotions, and habits. Most of us never get handed this kind of instruction book. In fact, traditional education skips over the subject of self-knowledge entirely. Life rarely gives us pop quizzes on understanding ourselves, yet this is the very foundation of mental health and resilience.
At Harvard Medical School, psychiatry education is evolving. Harvard-trained clinicians now blend rigorous science with practical insight from real lives—including their own mistakes and struggles. This approach goes beyond textbooks and research papers. It’s about learning from experience, both in the clinic and in life.
From Struggle to Self-Discovery: Dr. K’s Journey
Take Dr. K, for example. His story isn’t the typical straight line you might expect from a Harvard psychiatrist. In his own words (3.39-3.41), “the experience that I draw on is my own.” He struggled in high school and college, eventually failing out. Video game addiction took over, and he had no idea what he wanted to do with his life (3.44-3.50).
At 21, Dr. K traveled to India to find himself (3.50-3.55). He spent seven years studying to become a monk, immersing himself in ancient traditions like meditation. These practices, once considered mystical, are now validated by neuroscience research. Meditation, for example, has been shown to change brain structure and function, supporting emotional regulation and resilience.
But Dr. K didn’t stop there. He was skeptical, curious about what was really happening in the brain during these spiritual experiences (3.59-4.14). This curiosity led him to neuroscience research, and eventually to medical school. “The brain exists within the body,” he realized (4.24-4.33), so understanding mental health meant looking at the whole person. He became a psychiatrist because, as he puts it, “the mind was my favorite organ” (4.36-4.41).
Blending East and West: Science Meets Spirituality
This fusion of clinical, academic, and lived wisdom is at the heart of modern psychiatry education at Harvard. Ancient wisdom traditions like meditation and mindfulness are now supported by neuroscience. Research shows that these practices can help regulate mood, reduce anxiety, and even change the way your brain responds to stress.
Harvard psychiatrists, such as Dr. Chris Palmer, also emphasize the role of diet and metabolism in mental health. Studies indicate that diets high in sugar and ultra-processed foods can disrupt metabolic health, increasing the risk for depression and other mental disorders. The health of your gut microbiome, for example, can affect your mood and behavior—a reminder that mind and body are deeply connected.
Why Self-Reflection Matters More Than Achievement
Most people focus on external achievements—grades, jobs, accolades. But as Dr. K’s journey shows, it’s self-understanding that underpins true happiness and resilience. Self-reflection, not rote memorization, is the missing piece in most people’s lives. The journey from confusion to clarity isn’t linear, and it often gets messy. But that’s where real growth happens.
“The work that I do is on that whole continuum of pathology … But then going from negative 100 to zero is what medicine does…and from zero to positive 100 is when we really draw on spiritual traditions.” – Dr. K
True healing and self-mastery aren’t about perfection. They’re about building practical, honest self-knowledge—learning to read your own manual, one page at a time.
FAQ: Rethinking Psychiatry, Diagnosis, and Self-Improvement
What’s a “treatment-resistant” illness and why does it matter?
You might hear the term treatment resistant illness in psychiatry, especially when standard therapies—like medication or talk therapy—don’t seem to help. This isn’t rare. In fact, research shows that many people with depression, anxiety, or other mental health disorders don’t respond to first-line treatments. Harvard psychiatrists and global mental health leaders are sounding the alarm: as mental illness rates rise worldwide, the number of people struggling with treatment-resistant conditions is growing too. This matters because it pushes psychiatry education and neuroscience research to look for new answers—sometimes outside the traditional medical model.
Do diets and gut health really impact my mental well-being?
Absolutely. The link between diet and mental health is now a major focus in modern psychiatry research. Studies indicate that diets high in sugar and ultra-processed foods can disrupt metabolism and gut health, increasing your risk for depression, anxiety, and even ADHD. Harvard’s Dr. Chris Palmer and others are at the forefront, showing how the gut microbiome—those trillions of bacteria in your digestive tract—can affect your mood, motivation, and behavior. If you’ve ever felt “off” after a junk food binge, you’re not imagining it. Improving your diet and supporting gut health may be as important as therapy or medication for some people.
Can you rewire your brain after years of negative thinking?
Yes—thanks to neuroplasticity. Even if you’ve spent years stuck in negative thought patterns, neuroscience research confirms that your brain can change. This is the science behind many modern therapies and mindfulness practices. Dr. K, drawing from both Harvard psychiatry education and spiritual wisdom, explains that emotional habits aren’t fixed. With the right approach—like journaling, meditation, or even certain physical activities—you can strengthen new, healthier neural pathways. It’s not about “thinking positive” all the time, but about gently retraining your brain to respond differently over time.
How can men and women approach self-improvement differently without missing out on each other’s strengths?
There’s no one-size-fits-all answer, but gender differences in mental health are real. About 70% of psychotherapy patients and therapists are women, and research suggests that emotional awareness is often higher in women due to both biology (like estrogen) and social conditioning. Men, on the other hand, may be more likely to seek external solutions to internal problems—sometimes missing the value of emotional processing. Dr. K points out that the most successful people, regardless of gender, combine emotional intelligence (EQ) with practical action. Recognizing these differences can help you learn from others’ strengths rather than compete or compare.
Is there a single best approach—science, spiritual wisdom, or something else?
If you’re looking for a magic formula, you won’t find it. The most effective mental health strategies often blend science, spiritual traditions, and lived experience. Harvard psychiatry education emphasizes evidence-based care, but even top researchers acknowledge the value of practices like meditation, yoga, and self-reflection. Dr. K’s journey—from neuroscience research to monastic life—shows that healing and growth are rarely linear. Sometimes, the best teacher is life itself, especially when you’re willing to ask the right questions and stay curious about your own mind.
Conclusion: Unlocking Your Internal Change—One Honest Reflection at a Time
If you’ve made it this far, you know that the journey toward better Mental Health is anything but simple. The lessons from Harvard Psychiatry and the wisdom of life’s unlikely teachers both point to a single truth: real, lasting change starts from within. Surface-level fixes—those quick hacks or viral trends—might offer a momentary lift, but they rarely outsmart the deep-seated issues that shape your experience. Instead, true Internal Change asks for something more honest: a willingness to pause, reflect, and look beneath the surface.
Science and ancient traditions both have a place in your self-understanding toolkit. Harvard Psychiatry has shown us, through decades of research and clinical work, that the roots of mental health are complex. They’re woven from biology, psychology, social context, and even diet. For example, research shows that hormonal fluctuations can directly impact emotions—think of how premenstrual dysphoric disorder or PMS can cause real, felt shifts in mood and energy (12.37-12.49). These aren’t just “in your head.” They’re physical, chemical, and deeply human. At the same time, ancient practices like mindfulness, journaling, or simply sitting with your thoughts can help you notice patterns and stories that science alone can’t always explain.
It’s tempting to chase labels and diagnoses, especially when social media makes it seem like everyone has a quick answer. But careful evaluation matters far more than TikTok trends. Harvard Psychiatry reminds us that while labels can help you understand your challenges, they aren’t the whole story. You are more than a diagnosis. You are a person, with a unique internal narrative that deserves careful attention and respect.
Here’s the wrap-up wisdom: you’re not broken. You might just need a new approach, a little patience, and a willingness to look within. Studies indicate that many psychiatric treatments don’t work for everyone, and that’s not a personal failure—it’s a call for deeper exploration. Sometimes, the answer lies in unexpected places: a shift in diet, a new way of moving your body, or a conversation that helps you see yourself differently. Harvard psychiatrists like Chris Palmer are now exploring the links between metabolism, gut health, and mental well-being, showing that the mind and body are more connected than we once thought.
So, next time you feel the urge to chase a quick fix, pause. Ask yourself what your internal story is trying to teach you. Maybe it’s time to blend the best of science and self-reflection, to honor both the data and your lived experience. The global mental health movement, with roots in Harvard’s Department of Global Health and Social Medicine, is proof that hope and progress are possible—even when the path is uncertain.
In the end, unlocking your own internal change isn’t about perfection. It’s about honest reflection, a willingness to learn, and the courage to keep going—one step, one insight, one honest moment at a time.
TL;DR: Transformation starts inside: quick fixes and surface-level hacks rarely solve deep mental health struggles. Instead, blend internal exploration, scientific insight, and honest support to unlock real change. (Bonus tip: Don’t drown your problems in sugar—or TikTok diagnoses.)
Hats off to The Diary Of A CEO for their thought-provoking content! Take a look here: https://youtu.be/P1ALkQMfkjc?si=zev8bkW-dr1T8FqQ.