Confession time: I always thought my daily glass of wine was harmless—a personal ritual that kept stress at bay. Turns out, I might’ve been wrong. Did you know that what most of us consider ‘moderate’ drinking actually bumps up our cancer risk? It shocked me too, especially when I learned just how common addiction is, and how rarely we see it coming. Let’s dig into some facts and real stories that might just leave you rethinking your next pour.
1. Shattering the Moderate Drinking Myth: Why Less Isn’t Necessarily Safe
When you think about moderate drinking, what comes to mind? For many, it’s the image of a single glass of wine with dinner—harmless, maybe even healthy. But research shows that the dangers of moderate drinking are much greater than most people realize. The idea that “less is safe” is one of the most persistent myths in our culture, and it’s time to take a closer look at the real risks.
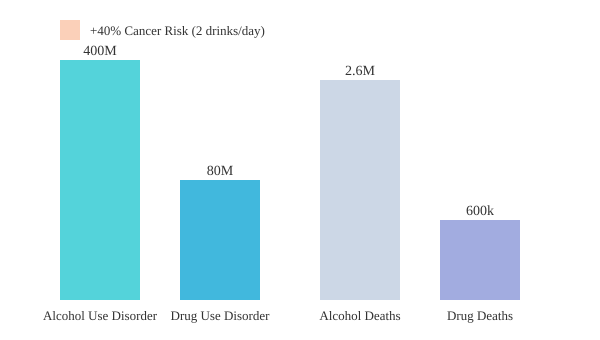
Let’s start with the numbers. According to Dr. Sarah Wakeakeman, a Harvard addiction expert, drinking just one glass of wine a day already puts you in the moderate risk category for health problems. That’s not just a vague warning—this level of alcohol intake is linked to an increased risk for nearly every form of cancer. If you add a second glass, the risks climb even higher. In fact, studies indicate that two glasses of wine per day can increase your cancer risk by about 40%. Even what’s considered “modest” drinking—well within what many see as normal—raises the risk of breast cancer by 5%.
Here’s a quick look at the data:
| Alcohol Intake | Risk Level | Health Impact |
|---|---|---|
| 1 glass/day | Moderate risk | Associated with most forms of cancer |
| 2 glasses/day | Heavy drinking | ~40% increased cancer risk |
| Moderate intake | Low to moderate risk | +5% breast cancer risk |
The numbers are clear, but the message hasn’t reached everyone. There’s a lot of misinformation out there about how much alcohol is “safe.” For years, you might have heard that a daily glass of red wine could protect your heart or even extend your life. However, Dr. Wakeakeman points out that these beliefs were based on flawed studies—ones that didn’t account for other factors like diet, exercise, or socioeconomic status. The latest research on alcohol and cancer risk makes it clear: there is no truly safe level of alcohol consumption.
It’s easy to underestimate the dangers of moderate drinking because it’s so normalized. Maybe you have a ritual—a glass of wine to unwind after work, a beer with friends, a cocktail at a celebration. These habits feel harmless, even comforting. But the science tells a different story. As Dr. Wakeakeman puts it,
‘If I have this glass of wine every day, you’d be in what we call moderate risk, which is associated with pretty much every form of cancer.’
What’s striking is how quickly risk adds up. You might think, “I’m healthy, I exercise, I eat well—surely a drink or two won’t hurt.” But the threshold for harm is lower than you think. For many, the idea that even small, daily amounts of alcohol carry significant health risks comes as a shock. It certainly did for me. I used to feel immune, convinced that my habits were normal and safe—until I saw the data.
So, why does this myth persist? Cultural norms, personal routines, and widespread misinformation all play a part. It’s easier to believe that moderate drinking is harmless than to face the uncomfortable reality. But understanding the real risks is the first step toward making informed choices about your health. The dangers of moderate drinking aren’t just theoretical—they’re real, measurable, and closer to home than you might think.
2. The Hidden Reach of Addiction: It’s Not Just ‘Other People’
When you think about addiction, it’s easy to imagine it as something that happens to “other people.” But research in addiction science paints a very different—and much closer to home—picture. In fact, one in three people may have a problem with alcohol at some point in their lives. That’s not a distant statistic. It’s your friends, your family, your colleagues, and maybe even you.
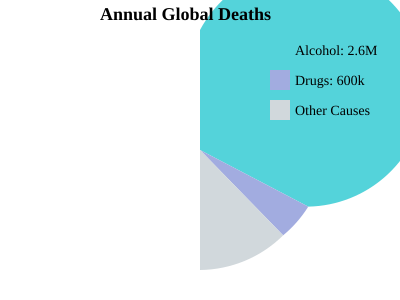
Globally, the numbers are staggering. Around 400 million people struggle with alcohol use disorder, and another 80 million grapple with other drug addictions. Each year, 2.6 million people die from alcohol-related causes. That’s about 7,000 people every single day. For drug-related deaths, the annual toll is 600,000—or roughly 1,600 lives lost daily. These alcohol-related deaths statistics are more than just numbers; they represent real people, real families, and real communities.
Yet, despite the scale, addiction often remains hidden. Stigma is a powerful silencer. Families keep secrets. Friends look the other way. The result? Addiction is far more common than most people are willing to admit. Studies indicate that nearly every family is touched by addiction in some way, whether they realize it or not. The silence around substance use only amplifies its impact, making it harder for those affected to seek help or speak openly.
I remember the moment it hit me personally. A close friend—always the life of the party, always “just having fun”—confided in me about their struggles with alcohol. At first, I thought it was an exception, a rare case. But as I listened and learned, I realized their story was part of a much wider pattern. The more I talked to others, the more I saw how common these battles really are. Addiction isn’t an outlier; it’s woven into the fabric of everyday life.
‘One in three people may have a problem with alcohol at some point in their lives.’
What makes addiction so widespread? Addiction science shows it’s not just about willpower or bad choices. Genetics play a major role, accounting for 40–60% of addiction risk. Trauma, especially adverse childhood experiences, is another powerful driver. The COVID-19 pandemic only made things worse, with increased isolation and stress leading to more substance use and higher death rates.
The impact of addiction isn’t limited to those who use substances. It ripples outward—affecting families, workplaces, and entire communities. And because of stigma, many people suffer in silence, believing they’re alone or that their situation is unique. But the facts say otherwise: substance abuse facts reveal that addiction is a widespread, deeply human issue.
So, the next time you hear about addiction, remember: it’s not just “other people.” It’s all of us. The science, the statistics, and the stories all point to the same truth—addiction is everywhere, and it thrives in the shadows of stigma and silence.
3. Anatomy of an Addiction: How Trauma, Genes, and Brain Chemistry Collide
When you think about addiction, it’s easy to imagine it as a personal failing or a simple matter of willpower. But research shows that the roots of addiction are far more complex, woven from your genetic code, your lived experiences—especially trauma—and the way alcohol interacts with your brain’s chemistry. Understanding this interplay is essential if you want to grasp why trauma and addiction are so closely linked, and why some people are more vulnerable than others.
Genetics: The 40–60% Factor
Let’s start with your genes. Studies indicate that about 40–60% of your risk for addiction is genetic, a number surprisingly similar to the genetic risk for diabetes. If you have a family history of substance use disorders, your odds of developing one yourself are higher. But genes aren’t destiny—they’re just one piece of the puzzle.
Trauma: The Real “Gateway Drug”
Now, consider the role of trauma. Dr. Sarah Wakeakeman, a Harvard addiction expert, puts it bluntly:
“Trauma is probably the single biggest driver. So, you often hear things like cannabis is a gateway drug. I would say trauma is the gateway drug.”
Research from the Adverse Childhood Experiences Study (ACES) shows a clear, linear relationship: the more traumatic events you experience as a child, the higher your risk for substance use later in life. This connection is so strong that childhood trauma substance use is now a major focus in prevention and treatment efforts. Trauma doesn’t just make you more likely to try substances—it changes how your brain responds to them, making addiction more likely.
Dopamine and Addiction: How Alcohol Hijacks Your Brain
Alcohol doesn’t just affect your mood. It targets multiple systems in your brain. When you drink, alcohol boosts dopamine (the “reward” chemical), increases GABA (which calms anxiety), and triggers the release of endogenous opioids (your body’s natural painkillers). This powerful cocktail makes alcohol feel rewarding and soothing—at least at first. Over time, your brain adapts, and you may find yourself drinking more just to feel “normal.” This is the core of dopamine and addiction: the brain’s reward system gets rewired, making it harder to stop even when you want to.
Alcohol’s Toll: Aging the Brain
The consequences of chronic alcohol use go far beyond hangovers. Brain scans reveal that a 43-year-old with a long history of heavy drinking can have a brain that looks like that of a 90-year-old with dementia. Alcohol accelerates brain aging, shrinking key areas involved in memory, decision-making, and emotional control. It’s a stark reminder that addiction is not just about pleasure—it’s about long-term harm to your body and mind.
Dependence vs. Addiction: The Coffee Question
You might wonder: if you crave coffee every morning, is that addiction? Not quite. Physical dependence (like needing caffeine to avoid a headache) is different from addiction, which is defined by continued use despite negative consequences. Addiction involves loss of control, compulsive use, and craving—often driven by deeper issues like trauma or genetic vulnerability.
| Key Factor | Research Insight |
|---|---|
| Genetic Risk | 40–60% of addiction risk is genetic |
| Trauma | ACES study: risk rises with number of childhood traumas |
| Brain Aging | 43-year-old with alcohol damage can have brain of a 90-year-old |
In short, addiction is not a simple story. It’s a collision of trauma, genes, and brain chemistry—one that can affect anyone, regardless of background. Recognizing these factors is the first step to understanding, compassion, and effective support.
4. The Pandemic Effect: When the World Stopped, Addiction Rates Surged
When the COVID-19 pandemic swept across the globe, it didn’t just disrupt routines and isolate communities—it triggered a dramatic shift in US alcohol use trends and substance-related deaths. Almost overnight, the world saw a surge in alcohol and drug use, with consequences that still ripple through society today.
Research shows that the pandemic was a powerful driver behind a sharp increase in addiction and related mortality. In the United States, alcohol-related deaths spiked by a staggering 23% immediately following the onset of the pandemic in March and April 2020. As Dr. Sarah Wakeakeman, Harvard addiction expert, put it:
“Immediately following the onset of the pandemic… we saw a 23% increase in alcohol-related mortality and… the highest rates ever we’ve seen of drug-related overdose deaths.”
This statistic is more than just a number. It represents thousands of lives lost, families upended, and communities left reeling. The spike in alcohol-related deaths statistics was mirrored by a record-setting rise in drug overdose deaths, marking the highest rates ever recorded in the US. While exact numbers for overdose deaths during this period are still being analyzed, the trend is clear: the pandemic and addiction became deeply intertwined.
Life Expectancy Drops: A Sobering Indicator
One of the most telling consequences of these trends is the drop in US life expectancy. Studies indicate that, compared to other wealthy nations, the United States experienced a much sharper decline in life expectancy during the pandemic years. Substance-related deaths—particularly those tied to alcohol and drugs—were a major factor. This is a stark reminder that the health impact of the pandemic extended far beyond the virus itself.
Who Was Hit Hardest?
Not everyone was affected equally. Frontline workers and caregivers, already under immense stress and pressure, faced some of the highest increases in substance use. The emotional toll of caring for others during a global crisis, combined with isolation and uncertainty, pushed many toward alcohol and drugs as coping mechanisms. For these individuals, the risk of developing addiction soared.
- Frontline workers: Nurses, doctors, and essential staff reported higher rates of substance use.
- Caregivers: Those supporting vulnerable family members or patients were especially at risk.
‘Drinking to Cope’—A Normalized Response?
During lockdown, “drinking to cope” became a common, almost normalized, response to stress and boredom. Social media was filled with jokes about “quarantinis” and wine o’clock, but the reality was far less lighthearted. Research into US alcohol use trends during this period reveals that increased drinking wasn’t just a harmless pastime—it came at a significant cost to physical and mental health.
For many, what started as a way to manage anxiety or fill empty hours quickly escalated. The line between moderate and risky drinking blurred, especially as routines disappeared and support systems fractured. The normalization of alcohol as a coping tool masked the real dangers, contributing to the surge in alcohol-related deaths statistics.
Pandemic and Addiction: Lessons Learned
The pandemic’s impact on addiction is a sobering lesson in how quickly circumstances can shift public health trends. When the world stopped, addiction rates surged—reminding us that substance use is deeply connected to stress, trauma, and social isolation. As we reflect on these years, it’s clear that understanding and addressing the drivers of addiction is more urgent than ever.
5. Busting Myths: Redefining Addiction Beyond ‘Bad Choices’
When you think about addiction, what comes to mind? For many, the first thought is often about personal responsibility—a belief that addiction is simply the result of bad choices or weak willpower. But addiction science tells a very different story. Understanding the true addiction definition is crucial, not just for those affected, but for everyone who wants to help reduce stigma and support recovery.
Let’s start with the basics. Addiction isn’t a moral failure. It’s not about lacking discipline or being “bad.” Instead, addiction is a complex health condition, shaped by genetics, trauma, and environment. The most accepted addiction definition in the field is based on the Four C’s:
- Loss of Control over substance use or behavior
- Compulsive use—feeling driven to use, even when you don’t want to
- Continued use despite Consequences—persisting even as relationships, health, or work suffer
- Craving—intense urges or preoccupation with the substance or behavior
As Dr. Sarah Wakeakeman, a leading voice in addiction science, explains:
“Addiction is really defined by use despite consequences. So continuing to do something in your life despite bad things happening to you because of it.”
This means that addictive behavior isn’t just about how often you use a substance or how much you enjoy it. It’s about what happens when you try to stop, and whether you keep going even as negative fallout piles up. Substance abuse facts show that addiction can affect anyone—regardless of background, education, or income.
Unfortunately, society often clings to the “bootstraps” mentality—the idea that people should just try harder, tough it out, or hit “rock bottom” before seeking help. Research shows this mindset actually delays treatment and makes outcomes worse. Shame and stigma are powerful barriers. When people feel judged or blamed, they’re less likely to reach out, and more likely to suffer in silence.
The medical model of addiction, supported by decades of research, makes it clear: addiction is not a weakness. It’s a chronic, relapsing condition that changes the brain’s reward system, decision-making, and self-control. Genetics play a major role—up to 60% of addiction risk is inherited. Trauma, especially adverse childhood experiences, further increases vulnerability. This is why two people can drink the same amount, but only one develops a problem.
Personal stories highlight the real-world impact of stigma. Dr. Wakeakeman herself was moved to action after seeing a loved one shamed instead of helped. That experience sparked a realization: compassion, not judgment, is what truly supports recovery. Science-based interventions—like medication, therapy, and social support—are much more effective than punishment or “tough love.”
Changing the language we use is another important step. Terms like “substance abuser” or “dirty” reinforce shame and make it harder for people to seek help. Instead, using person-first language—such as “person with addiction” or “person in recovery”—can make a real difference. Research indicates that understanding the modern addiction definition helps fight stigma and encourages more people to access the care they need.
In summary, addiction is not about “bad choices.” It’s a medical condition defined by the Four C’s: loss of control, compulsive use, continued use despite consequences, and craving. The more you understand the science, the better equipped you are to support those affected—and to challenge the myths that keep so many from getting help.
6. The Medical System’s Silo Problem: Why Effective Addiction Care Is Still Rare
When you think about addiction treatment models, you might picture specialized rehab centers or support groups, often operating outside the walls of mainstream hospitals. This separation isn’t just a matter of logistics—it’s a fundamental flaw in how our healthcare system addresses addiction. The result? Gaps in care, missed opportunities for intervention, and poorer outcomes for millions struggling with substance use disorders.
Dr. Sarah Wakeakeman, a Harvard professor and addiction expert, puts it plainly: “My mission is really to change the way people think about and understand alcohol and drug problems and also to give people the evidence and the facts both to understand addiction.” Her work at a major academic medical center focuses on breaking down these silos, advocating for the integration of addiction care into the broader medical system. This shift is crucial—not just for patients, but for the healthcare system as a whole.
Why does this silo exist? Historically, addiction has been viewed through a moral lens, treated as a “bad habit” rather than a chronic medical condition. Imagine if we treated a broken leg with lectures about willpower instead of a cast and physical therapy. The analogy isn’t far-fetched. When addiction is addressed as a behavioral flaw, people are less likely to receive the evidence-based rehab and medical interventions that research shows can truly make a difference.
Most rehab programs in the United States still don’t offer treatments that target the brain’s opioid response—the very system hijacked by substances like alcohol and drugs. Instead, many facilities rely on unproven therapies, while effective medications (such as those that block alcohol’s painkiller effects) remain underutilized. This lack of access to evidence-based tools leaves many patients cycling through relapse and recovery, never receiving the comprehensive care they need.
There’s a growing recognition that integration of addiction care within mainstream medicine is essential. Studies indicate that when addiction treatment is woven into primary care, emergency departments, and specialty clinics, patient outcomes improve dramatically. This means fewer overdoses, lower rates of relapse, and better overall health. Yet, the path to this integration is slow, in part because most doctors receive little training in addiction medicine.
Programs like Harvard’s addiction medicine fellowship are working to change this. By training physicians to recognize, diagnose, and treat substance use disorders with the same rigor as diabetes or heart disease, these initiatives are laying the groundwork for a new generation of healthcare providers. The goal is simple: make evidence-based rehab and treatment models the standard, not the exception.
It’s worth noting that medications can play a powerful role in recovery. For example, drugs that block the brain’s opioid receptors can reduce the rewarding effects of alcohol, making it easier for people to cut back or quit. But without integration into routine care, these options remain out of reach for many. The unequal and often separate nature of addiction care means that only a fraction of those who need help actually receive it.
Ultimately, treating addiction like any other medical condition—using science, compassion, and proven interventions—offers the best chance for recovery. As Dr. Wakeakeman’s work highlights, bringing addiction care back into the medical mainstream is not just a professional focus; it’s a necessary evolution in how we understand and address one of society’s most pressing health challenges.
7. Rethinking Recovery: From Isolation to Connection
If you’ve ever wondered what truly helps people heal from addiction, it may surprise you to learn that the answer isn’t just sobriety. It’s connection. As Dr. Sarah Wakeakeman, a leading voice in addiction medicine, puts it:
‘We often talk about the opposite of addiction is not sobriety, it’s actually connection.’
This idea is more than just a catchy phrase—it’s a research-backed insight that’s changing how we approach addiction recovery support and trauma-informed care.
Let’s break this down. Addiction, whether to alcohol, drugs, or even behaviors like gambling or social media, tends to flourish in isolation. When you’re cut off from support, community, and meaningful relationships, substances or compulsive behaviors can fill that void. During the COVID-19 pandemic, for example, rates of alcohol-related deaths jumped by 23%. Loneliness, boredom, and trauma all played a role. It’s not just about the substance—it’s about what’s missing from your life.
Trauma is a big part of this story. As Dr. Wakeakeman explains, trauma isn’t just about what happened to you—it’s about being left alone to deal with it. When people are isolated with their pain, addiction can become a way to cope. But the flip side is just as powerful: healing often starts when you feel like you belong, when you’re seen and supported. That’s the heart of trauma-informed care—recognizing that recovery is about rebuilding trust, safety, and connection, not just eliminating a substance.
Research shows that social connection is foundational for addiction prevention and recovery. The famous “Rat Park” experiment illustrated this perfectly: rats kept in isolation chose drugs over food, but when placed in a stimulating, social environment, their drug use dropped dramatically. Humans aren’t so different. When you have strong social supports—friends, family, community groups—your risk for addiction drops, and your chances of recovery soar.
Imagine if every workplace offered weekly “connection hours” instead of just happy hour. What if, instead of centering social events around alcohol, we focused on building real relationships and support networks? It’s a wild card idea, but it gets at the heart of what’s missing in many people’s lives. Social rituals don’t have to revolve around drinking—they can be about genuine connection.
Sometimes, the most powerful addiction recovery support you can give isn’t advice or intervention. It’s simply being there. The best support I ever gave a friend was just sitting and listening. No judgment, no solutions—just presence. That’s often what people struggling with addiction need most: someone who will sit with them in their pain, not try to fix it or push them away.
Over time, these small acts of connection can replace the reliance on substances. Healing doesn’t happen in a vacuum. It’s a process that unfolds in community, through relationships, and with the support of others who care. If you’re thinking about your own recovery, or supporting someone else, remember: you don’t have to do it alone. Connection is not just a nice-to-have—it’s the foundation of lasting change.
8. Table Time: Key Stats on Alcohol, Addiction, and Mortality
When you look at the numbers behind alcohol and addiction, the scale is both sobering and urgent. Research shows that visualizing these statistics can truly bring home the reality—this isn’t just a distant issue, but one that touches nearly every family, workplace, and community. Let’s break down the most important substance abuse facts and alcohol-related deaths statistics to give you a clear, science-based snapshot of where things stand today.
Globally, alcohol use disorder affects an estimated 400 million people. That’s nearly the population of the United States and Canada combined, living with a condition that can quietly erode health, relationships, and futures. Drug use disorders, while less common, still impact 80 million people worldwide. These numbers aren’t just statistics—they represent real lives, families, and stories.
The mortality figures are even more striking. Each year, 2.6 million people die from alcohol-related causes around the world. That’s about 7,000 deaths every single day. In comparison, drug-related deaths account for 600,000 lives lost annually, or roughly 1,600 people per day. These alcohol-related deaths statistics highlight how alcohol, often seen as a “social” or “normal” substance, is responsible for more deaths than all illicit drugs combined.
But it’s not just about the numbers—it’s about the risks that come with even what many consider “moderate” drinking. Studies indicate that drinking two glasses of wine per day increases your risk of developing certain cancers by 40%. Even at lower levels, such as one glass per day, there’s a measurable increase in breast cancer risk (about 5%), and research now shows that no amount of alcohol is truly “safe” for your health. The COVID-19 pandemic only made things worse, with a 23% spike in alcohol-related mortality after early 2020, as loneliness, trauma, and stress drove more people toward risky drinking patterns.
To help you visualize these addiction science findings, here’s a comparison chart that distills the core data:
These numbers aren’t meant to scare you, but to inform and empower. Maybe you’re surprised to learn that your own birth year falls within an era of rising risk, or that the pandemic years saw such a dramatic spike. The point is: addiction and alcohol-related harm aren’t abstract—they’re woven into the fabric of our society, and understanding the scale is the first step toward change.
As you reflect on these substance abuse facts, remember that addiction is not a moral failing. It’s a complex, science-backed condition influenced by genetics, trauma, and environment. The urgency in these statistics isn’t just about numbers—it’s about the lives behind them, and the hope that comes from recognizing addiction as a treatable, preventable health issue. By staying informed and compassionate, you can be part of a smarter, kinder response to one of the most pressing public health challenges of our time.
TL;DR: Drinking even small amounts of alcohol raises your risk for serious health problems, and addiction can touch anyone. Genetics, trauma, and misinformation all play a role. Understanding the science can help us make better choices and support those struggling.
Hats off to The Diary Of A CEO for the valuable insights! Take a look at it here: https://youtu.be/Fg7U-BhiZGE?si=mzDOYGA2fn782NR8.