Picture this: You wake up groggy, already dodging anxiety before your feet hit the floor. Most of us shrug this off as ‘just life.’ But what if the problem was hiding in your breakfast bowl, not your DNA? Years ago, after a midday crash so profound I almost napped under my desk (true story!), I realized my food was making me foggy, not just sleepy. Little did I know, a seismic shift in brain nutrition was about to flip how I—and plenty of experts—view mental wellness. Let’s question everything you think you know about eating for your mind.
1. The Ketogenic Diet: Hope or Hype for Mental Health?
If you’ve ever wondered whether what you eat could truly impact your mind, you’re not alone. For decades, the mainstream approach to mental health has focused almost exclusively on medication and therapy. But what if a major dietary shift—specifically, the ketogenic diet—could rapidly improve or even remit severe mental illness? Let’s take a closer look at what research and real-world experience are revealing about the ketogenic diet mental health connection.
How Fast Can Diet Change Your Mind?
It might sound surprising, but studies indicate that many people experience significant reductions in anxiety within just 3 days to 3 weeks of starting a ketogenic diet (0.00-0.04). That’s a remarkably short time frame, especially when compared to how long psychiatric medications can take to show results. The rapid onset of relief is one of the reasons more clinicians and patients are taking notice.
Clinical Remission: The Numbers Speak
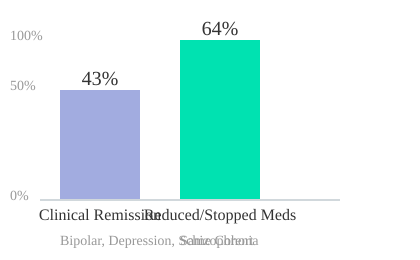
A pivotal study led by Dr. Georgia Ede, a psychiatrist and nutrition specialist, explored the effects of a ketogenic diet on patients with some of the most challenging psychiatric diagnoses: bipolar disorder, major depression, and schizophrenia (0.06-0.09). The results were striking. In this group, 43% achieved clinical remission from their chronic mental illness (0.11-0.15). That means nearly half of the participants saw their symptoms resolve to the point where they no longer met criteria for their diagnosis.
Even more compelling, 64% of these patients were able to reduce or completely eliminate their psychiatric medications after making the dietary change. For those who have struggled with side effects or incomplete relief from medications, these numbers offer a new sense of hope.
Beyond Medication: Food as a Powerful Tool
Most people expect drugs, not food, to change the brain. But research shows that nutrition strategies can sometimes succeed where medicine falls short—and often, the results come surprisingly quickly. The ketogenic diet, by shifting the body’s primary fuel source from carbohydrates to fats, appears to influence brain chemistry in ways that support mental stability and resilience.
Dr. Georgia Ede, who has worked with patients struggling with severe mental illnesses, puts it this way:
People need to know how powerful nutrition strategies can be for the brain because if you’re feeding it the wrong way, things will go wrong. – Dr. Georgia Ede
When “Healthy” Isn’t Enough: A Personal Perspective
It’s easy to assume that eating a standard “healthy” diet—low in fat, high in whole grains, lots of fruits and vegetables—should be enough to support mental health. But for some, these mainstream recommendations don’t deliver the relief they’re seeking. There are countless stories of individuals who tried every conventional approach, only to find real improvement when they went against the grain—literally—by embracing a ketogenic or low-carb approach.
Why the Ketogenic Diet Mental Health Connection Matters
The evidence is mounting: a mental illness remission diet like the ketogenic diet isn’t just hype. For a significant proportion of people with conditions like bipolar disorder, depression, or schizophrenia, it can be a game-changer. Relief may come in days or weeks, not months or years. If you’re searching for answers, it may be time to rethink what’s on your plate.
2. What Causes Brain Chemical Imbalances? (Spoiler: It’s Not Just Your Genes)
If you’ve ever been told that your mental health struggles boil down to a “chemical imbalance,” you’re not alone. For decades, this idea has shaped how we think about depression, anxiety, and other mental health conditions. But what if the real story is much more complex—and, in some ways, far more hopeful? Let’s dig into what’s really behind those shifts in brain chemistry, and why metabolic psychiatry is turning heads in the world of mental health.
Beyond the Neurotransmitter Myth
You might have heard that mental illness is caused by mysterious imbalances in neurotransmitters like serotonin or dopamine. While these chemicals do play a role in mood and cognition, research shows that this explanation is overly simplistic. As Dr. Georgia Ede, a Harvard-trained psychiatrist specializing in nutritional psychiatry, points out (0.20–0.25), the real question is: What’s causing those chemical imbalances in the first place?
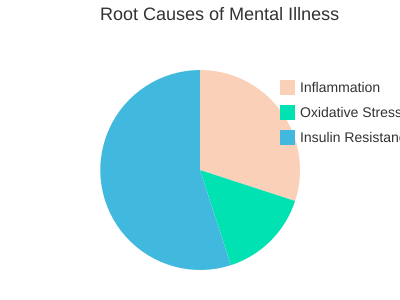
The Real Culprits: Inflammation, Oxidative Stress, and Insulin Resistance
Emerging science suggests that the root causes of brain chemical imbalances are not just genetic or random. Instead, three main factors stand out:
- Brain inflammation: Chronic inflammation can disrupt how your brain cells communicate, leading to mood swings and cognitive issues.
- Oxidative stress: This is when your body’s natural defense systems can’t keep up with damaging free radicals, which can harm brain cells and impair function.
- Insulin resistance: Surprisingly, up to 90% of Americans have some degree of insulin resistance or pre-diabetes (implied in transcript). This hidden metabolic issue is now recognized as a major risk factor for mental health problems.
These factors are at the heart of what’s now being called metabolic psychiatry—a new field that explores how metabolism and nutrition directly impact brain health.
Metabolic Psychiatry: A New Frontier
Metabolic psychiatry, a term championed by Dr. Shabani Sethi, is gaining momentum as researchers connect the dots between diet, metabolism, and mental health. This approach challenges the conventional wisdom that mental illnesses are purely chronic, mysterious, and incurable. As Dr. Ede puts it:
“We’ve been taught to think of mental illnesses as chronic, mysterious, and incurable… but we can do much more about them than we realize.” – Dr. Georgia Ede
By focusing on the underlying metabolic drivers—like inflammation and insulin resistance—metabolic psychiatry offers new hope for people who haven’t found relief with traditional treatments.
Why Nutrition Matters (and Why Most Doctors Don’t Know This)
One surprising fact: most psychiatrists receive less than 3–4 hours of nutrition education during their entire four years of medical school. Dr. Ede notes that nutrition is often overlooked in medicine due to this lack of training (0.30–0.34). That means many doctors are simply unaware of how powerfully food choices can affect brain chemistry and mental well-being.
Think of your brain as a high-performance engine. If you fuel it with the wrong foods—high in sugar, processed carbs, and inflammatory oils—things are bound to break down. But when you nourish it properly, you give your brain the best chance to function at its peak.
Visualizing the Root Causes
To better understand the primary drivers of mental illness, take a look at the chart below. It illustrates the relative impact of inflammation, oxidative stress, and insulin resistance—three key factors at the core of inflammation brain health research and metabolic psychiatry.
As you can see, the landscape of mental health is shifting. The focus is moving away from blaming your genes or mysterious chemicals, and toward addressing the metabolic roots—through nutrition, lifestyle, and a deeper understanding of how your body and brain are connected.
3. Outrunning Conventional Wisdom: When ‘Healthy’ Diets Fail You
If you’ve ever followed mainstream nutrition advice to the letter—loading up on whole grains, piling blueberries on your oatmeal, blending flaxseed smoothies, and cutting back on animal fats—only to feel your health and mood slipping, you’re not alone. The story is all too familiar, and it’s one that Dr. Georgia Ede knows firsthand. Her journey, and that of many of her patients, reveals a surprising truth: sometimes, the “healthiest” diets can actually lead to brain nutrition failure and worsening symptoms (0:47–1:25).
When Doing Everything “Right” Goes Wrong
For more than a decade, Dr. Ede followed the textbook approach to nutrition. She ate a low-fat, high-fiber, mostly plant-based diet, exercised religiously, and kept calories in check. Yet, by her early 40s, she found herself battling chronic fatigue, IBS, anxiety, and depression—symptoms echoed by many of her patients (0:49–0:57). Despite extensive testing from top specialists, she was told nothing was wrong. But she knew something was off.
This is a common scenario: you try every “healthy” eating trick in the book, but your mental health doesn’t budge. Maybe you’ve even felt frustrated or resigned, thinking, “I tried eating more whole foods, more plants, less fat, but nothing changed.” Dr. Ede’s experience reflects this widespread disappointment with conventional wisdom (8:13–8:59).
Why Most Nutrition Advice for Mental Health Falls Short
The problem, as Dr. Ede discovered, is that much of the advice aimed at nutrition and mood improvement is either incomplete or flat-out wrong (8:26–8:42). We’re taught to believe that mental illnesses are mysterious, chronic, and best managed with medication and therapy. Nutrition is rarely seen as a powerful tool for the brain. In fact, many are led to believe that food doesn’t matter much for brain health at all (7:19–8:18).
But research shows that the brain is highly responsive to what you eat. The catch? The mainstream recommendations—more plants, less animal food, low fat—often fail to resolve symptoms. In Dr. Ede’s case, and in the stories of many patients, improvement only came after abandoning these “rules” and exploring radically different dietary approaches.
Turning Mainstream Nutrition on Its Head
After years of feeling stuck, Dr. Ede began experimenting with her diet. Through trial and error, she found that the diet that finally resolved her symptoms was almost the opposite of what she’d been told was healthy. It was higher in fat, lower in carbs, and included more animal-based foods—an approach that, according to mainstream dogma, should have made things worse (1:04–1:10).
I tried everything correctly—low-fat, high fiber, whole foods. My health kept getting worse until I turned mainstream nutrition on its head.
This wasn’t just a personal revelation. Dr. Ede noticed similar patterns in her patients. Many had spent years following “perfect” diets, only to see their mental and physical health decline. It was only after they challenged the standard advice and tried unconventional strategies—like ketogenic or animal-based diets—that they saw real, lasting improvements (10:47–12:17).
Case Anecdotes: Breaking the Rules for Better Results
The stories are striking. Patients who had struggled with chronic fatigue, IBS, migraines, and mood disorders for years found relief not by doubling down on plant-based, low-fat diets, but by flipping the script. For some, this meant embracing high-fat, low-carb, or animal-based eating patterns. The improvements often came quickly—sometimes within days or weeks—and were more profound than any medication or therapy had delivered (9:11–9:32).
If you’ve been let down by mainstream nutrition advice, you’re not alone. The evidence—and the lived experience of many—suggests that nutrition and mood improvement often requires challenging the trends you’ve been taught to trust.
| Approach | Outcome |
|---|---|
| 10+ years of conventional practice/‘perfect’ diet | Noticeable health decline |
| Multiple failed attempts with standard whole foods approach | Persistent symptoms (fatigue, IBS, mood issues) |
The takeaway? Sometimes, the path to better brain health means questioning everything you thought you knew about “healthy” eating.
4. The Real-Life Transformation: Symptom Tracking and Diet Experiments
When it comes to mental health, most people rarely consider the food on their plate as a major factor. You might accept brain fog, chronic fatigue, or even anxiety as just part of life. But what if a few months of careful diet tracking could flip the script? This is exactly what happened in a real-life case that challenges everything we think we know about nutrition and mental well-being (11.49–12.56).
Discovering Surprising Triggers Through Diet Tracking
Imagine starting with a simple experiment: you keep a food and symptom journal for six months. Each day, you jot down what you eat and how you feel—physically and mentally. This process, while straightforward, can reveal patterns and triggers you never expected. In this case, the author began tracking out of instinct, not expecting much. But after half a year of trial and error, the results were nothing short of transformative.
| Duration | Method | Diet Type | Outcome |
|---|---|---|---|
| 6 months | Food & Symptom Journaling | Low-carb, high-fat, high-animal product (contradictory to health orthodoxy) | Significant relief from chronic fatigue, IBS, migraines, anxiety, depression |
The ‘Backwards’ Diet: Turning Conventional Wisdom Upside Down
What makes this story remarkable is the outcome. After months of tracking and tweaking, the diet that brought relief was almost the opposite of what most health guidelines recommend. Instead of focusing on whole grains, legumes, and plant-based foods, the author’s accidental solution was a mostly meat-based, low-carb, high-fat, and minimal fiber diet. Think seafood, meat, poultry, non-starchy vegetables, and animal fats—while minimizing grains and legumes.
This “backwards” approach not only resolved persistent physical health issues like chronic fatigue, IBS, and migraines, but also brought about a dramatic improvement in mental health. The author shares,
It improved my mental health significantly and I wasn’t even trying.
That’s the kind of accidental discovery that makes diet experiment success stories so compelling. You might start out trying to fix your stomach, only to find your mind feels clearer, your mood lifts, and those afternoon energy crashes fade away.
Diet Tracking and Mental Health: What the Research Shows
Research shows that diet tracking for mental health can help you identify surprising dietary triggers. Many people walk around with “normal” low mood, Sunday night anxiety, or daily slumps, not realizing these symptoms might be reversible with the right dietary changes. Studies indicate that, for some, a ketogenic diet can help with depression and anxiety, especially when traditional approaches haven’t worked.
In this real-world case, the transformation took just six months—a timeframe that’s both realistic and encouraging. It’s a reminder that improvements are possible in months, not years, when you approach your health as an experiment and listen to your body’s feedback.
How to Start Your Own Diet Experiment
- Track everything: Write down what you eat and how you feel each day. Be honest and detailed.
- Look for patterns: Notice if certain foods are followed by fatigue, mood dips, or digestive issues.
- Be open to surprises: The foods you think are “healthy” might not work for you. Trust your own data.
- Give it time: Real change took six months in this case. Be patient and persistent.
- Consult professionals: Especially if you have underlying health conditions, work with a healthcare provider familiar with diet and mental health.
Ultimately, tracking your symptoms and experimenting with your diet can lead to unexpected and life-changing results. Whether you’re struggling with depression, anxiety, or just want more energy and clarity, a few months of focused attention could reveal solutions you never imagined. The key is to stay curious, keep a journal, and be willing to challenge what you think you know about food and mental health.
5. Nutrition to Support, Not Replace, the Mind’s Machinery
When it comes to mental health, it’s easy to fall into the trap of looking for a single solution—a magic bullet that will fix everything. But the reality is, your brain is a complex, responsive organ that listens to much more than just what you eat (7.44–7.50). This is where the concept of holistic brain nutrition comes in. Nutrition is a powerful support for your mind’s machinery, but it’s not the only factor at play.
Let’s be clear: diet alone won’t solve every mental health challenge. Still, it can be the missing foundation that makes all the difference. Many people try to improve their mental health with therapy or medication, and those are important tools. But nutrition mental health support is often overlooked or misapplied, even though it can be just as crucial (7.52–7.56).
The Brain Listens to Everything
Your brain isn’t just paying attention to the food you eat. It’s also affected by how much sunlight you get, the love and support in your life, your job satisfaction, the people you spend time with, how much you move your body, and the amount of stress you experience (7.50–8.07). All these elements feed your brain in different ways. It’s a reminder that mental health is holistic. Poor nutrition is just one overlooked tool in a much bigger box.
Everything matters to the brain, but most people are led to believe that food doesn’t matter that much.
This quote from the source (8.08–8.14) captures a common misconception. Many people are told—directly or indirectly—that what they eat isn’t all that important for their brain. Part of the problem is that nutrition has only recently started to get attention in the context of mental health (8.14–8.20). And even then, the advice people receive is often outdated or just plain wrong (8.20–8.28).
When “Healthy” Diets Don’t Work
Maybe you’ve tried eating more whole foods, adding blueberries to your oatmeal, making flaxseed smoothies, or focusing on plant-based meals. These are all popular strategies, and they sound healthy. But for many people, these changes don’t lead to noticeable improvements in mood, memory, or concentration (8.28–8.57). It’s easy to get discouraged and think, “Maybe food just doesn’t matter for my brain.”
But here’s the twist: sometimes, what “shouldn’t” work—like high-fat, animal-based diets—can actually help when trendy diets fail. Research shows that for some individuals, especially those with treatment-resistant mental health issues, a ketogenic diet or similar approach can bring about meaningful improvements in days to weeks (9.11–9.32). It’s not about following the latest fad, but about finding what actually supports your unique brain.
Nutrition: The Overlooked Pillar
Despite its importance, nutrition is still not a major focus in mental health care. Did you know that psychiatrists receive less than 3–4 hours of nutrition training during four years of medical school? That’s a tiny fraction, considering how much what you eat can influence your mood, energy, and overall mental stability.
So, where does nutrition fit in? Think of it as the foundation—not the whole house—of mind health. It’s not about replacing therapy, medication, or other supports. Instead, it’s about giving your brain the raw materials it needs to function at its best. When you combine holistic brain nutrition with other pillars—like sunlight, community, sleep hygiene, and meaningful work—you create a much stronger base for mental wellness.
Looking Beyond the Plate
Ultimately, your brain’s health is shaped by a web of influences. Food is a key player, but so are the people you love, the work you do, the light you see, and the rest you get. If you’ve tried “healthy” diets without success, don’t give up. Sometimes, the answer lies in what you haven’t tried yet—or in rethinking what “healthy” really means for your mind. Nutrition is an overlooked pillar for mental wellness, but it’s not the only key. The best results come from a truly holistic approach.
6. Wild Cards: What If Your Brain’s ‘Normal’ Isn’t Normal?
Take a moment and ask yourself: What if the way you feel every day—your energy, your mood, your mental sharpness—isn’t actually “normal” at all? It’s a bold question, but it’s one that sits at the heart of the mental health self-experiment movement. We’re so used to hearing that things like midday fatigue, Sunday night dread, or that low-level anxiety are just part of life. But what if these aren’t inevitable? What if they’re actually nutritional red flags, quietly signaling that your brain’s needs aren’t being met?
Let’s dig into this idea with a simple thought experiment. Imagine if, instead of accepting subpar mental health as the baseline, you started to question it. What might you discover about yourself? According to the transcript (13.05-13.09), “all of these things we think of as really normal”—the winter blues, the constant tiredness, the brain fog—might not be normal at all. In fact, as the speaker puts it,
“We’ve come to expect so little of our mental health. We’ve come to expect poor mental health as normal—and it isn’t.”
(13.09-13.17)
Challenging the “Normal” Baseline
It’s easy to fall into the trap of believing that what’s common is what’s normal. But research shows that not all that is common is optimal; defaulting to the average sells ourselves short. Most people mistake chronic mild anxiety and fatigue as the baseline, not a solvable problem. The line between common and normal is worth questioning, especially when it comes to your brain health.
Consider how often you hear friends or coworkers complain about feeling drained by mid-afternoon, or dreading the start of the workweek. It’s so widespread that we rarely pause to ask: Is this just how life is, or could it be a sign that something’s off? Studies indicate that when people try non-conventional dietary tweaks—like a ketogenic diet—they sometimes report a dramatic shift in mental clarity, resilience, and mood stability. Suddenly, what they thought was “normal” turns out to be anything but optimal.
Why Do We Settle?
There’s a powerful quote from the transcript that sums up this dilemma:
“We’ve come to expect poor mental health as normal—and it isn’t.”
(13.14-13.17) It’s a wake-up call. Why do we settle for less when it comes to our mental health? Part of the answer may be habit. In a recent survey, about 53% of show listeners weren’t yet subscribed—suggesting how often we resist changing habits unless prompted. We get comfortable, even with discomfort, because it’s familiar.
Mental Health Self-Experiment: Dare to Question
Here’s where the concept of a mental health self-experiment comes in. What if you stopped accepting your current state as the best you can do? What if you tried something different—like adjusting your diet, your sleep, or your daily routines—and tracked the results? You might find that mental clarity, resilience, and a stable mood aren’t reserved for the genetically lucky. They’re available to anyone willing to experiment and challenge assumptions.
- Midday fatigue—not just a sign of a busy life, but possibly a nutritional imbalance.
- Sunday night dread—not inevitable, but potentially a sign your brain needs different fuel.
- Chronic mild anxiety—not your permanent baseline, but a solvable problem.
Opening up to non-conventional dietary tweaks, like a ketogenic diet, can unlock new self-understanding. It’s not about chasing perfection, but about recognizing that your “normal” might not be as fixed as you think. The difference between normal vs optimal brain health is often just a willingness to ask, “What if?”
So, next time you catch yourself settling for less, remember: We’ve come to expect so little of our mental health. We’ve come to expect poor mental health as normal—and it isn’t. (13.09-13.17)
7. Unexpected FAQ: The Burning Questions About Diet and Your Brain
When you start exploring the link between nutrition and mental health, it’s natural to have a lot of questions—some straightforward, others surprisingly complex. This ketogenic diet FAQ section is built on the real, sometimes quirky, concerns that come up in clinics and online communities. The truth is, mental health diet safety isn’t a one-size-fits-all topic. Research shows that answers are often nuanced, and what works for one person may not work for another.
Is ketogenic eating safe for everyone? This is probably the most common question, and for good reason. The short answer: not always. While many people benefit from a ketogenic diet, especially those with metabolic issues or certain psychiatric conditions, there are exceptions. For example, people with rare metabolic disorders, pregnant women, or those with a history of eating disorders should approach ketosis with extra caution and medical supervision. Dr. Georgia Ede emphasizes that safety comes down to your unique health status, medications, and even your psychological history. If you’re considering a major dietary change, especially for mental health, it’s wise to consult a knowledgeable healthcare provider.
How long does it take to notice changes? If you’re hoping for overnight miracles, you might be surprised. However, research and clinical experience suggest that some people see reductions in anxiety and improvements in mood within three days to three weeks of starting a ketogenic diet. Others may need more time, especially if underlying metabolic issues are significant. The adjustment period—sometimes called “keto flu”—can bring temporary discomfort, but this usually passes as your body adapts to burning fat for fuel.
Are there risks for people with certain conditions? Absolutely. People with type 1 diabetes, certain genetic disorders, or those taking specific medications (like insulin or psychiatric drugs) need close monitoring. The ketogenic diet can change how your body processes medications, sometimes requiring dose adjustments. Dr. Ede’s approach is careful and individualized, often involving a team that includes your doctor, a dietitian, and sometimes a therapist.
Can you combine therapy and dietary change? Yes—and in fact, it’s often the best approach. Nutrition can be a powerful tool, but it’s not a replacement for therapy, medication, or other supports when needed. Many people find that combining a brain-healthy diet with counseling or behavioral coaching leads to the most sustainable results. Dr. Ede recommends a team approach, especially during the first few weeks of dietary change, to help you navigate both the emotional and physical adjustments.
Should I go ‘cold turkey’ or ease into dietary overhauls? There’s no universal answer here. Some people thrive on jumping right in, while others do better with gradual changes. Research indicates that easing in—by slowly reducing carbohydrates and processed foods—can minimize side effects and make the transition more comfortable. Tracking your symptoms and progress can help you find the right pace.
What else should I track besides food? Food logs are helpful, but don’t stop there. Consider tracking your mood, sleep, energy, and even social interactions. These patterns can reveal how dietary changes are affecting your mental health. Affordable blood ketone meters can help you confirm when you’re in ketosis, but remember: numbers are just one piece of the puzzle.
Are plant-based and high-carb diets ever preferable? Why do they work for some but not others? This is where things get truly individual. While ketogenic diets have shown promise for many, some people genuinely feel better on plant-based or higher-carb diets. Genetics, gut health, activity level, and even cultural background can influence what works best for you. Dr. Ede’s philosophy is “nutritionally pro-choice”—meaning the best diet is the one that nourishes, protects, and energizes your brain, tailored to your unique needs.
In the end, the most important takeaway is that there are no simple, binary answers in the world of nutrition and mental health. Your journey may involve trial and error, support from a team, and a willingness to rethink what you thought you knew about food and your brain. As Dr. Ede reminds us, hope is always on the menu—and sometimes, the right question is the first step toward real change.
TL;DR: Stop blaming your brain chemistry. Diet—radically different from what you’ve been told—might make all the difference. The right nutrition strategy could trigger remission, improved moods, and greater clarity faster than expected.
A big shoutout to The Diary Of A CEO for delivering such insightful content! Be sure to check it out here: https://youtu.be/B7tnfSPySb0?si=RLIu2vEkOAYmt-hT.