Let me start with a confession: a few years ago, while scrubbing the kitchen floor at 8 p.m. (instead of, say, spending time with my partner or taking a walk), I realized something was off. I was exhausted, irritable, and somehow gaining belly fat despite chasing all the fitness trends. Turns out, I wasn’t alone. Most women I know—my aunt, my hyper-fit friend from college, even my yoga instructor—all whispered the same thing: ‘My body just… changed.’ So, why do so many of us accept sluggishness, stress, or hormonal havoc as the new normal? The truth is more complicated (and hopeful) than you’d think. In this post, we’re busting myths, facing the messy link between trauma and chronic disease, and exposing why mainstream medicine might not have your back. Let’s get genuinely curious about what makes you feel better—not just average.
Section 1: The Hidden Epidemic—Why 75% of Women Miss Out on the Care They Deserve (Table Inside)
If you’re like most women, you’ve probably wondered why your body feels different as you get older—why stress seems harder to manage, why stubborn belly fat appears out of nowhere, or why your interest in sex has faded. You’re not alone. According to recent findings, a staggering 3% to 75% of women do not receive the menopause care they truly deserve (0.00-0.03). That’s not a typo—the gap is massive, and it’s a hidden epidemic impacting women’s wellness everywhere.
Let’s break down what’s really happening. As you move through perimenopause and menopause, your body undergoes dramatic hormonal changes. Yet, most women are left to navigate this journey with little guidance or support. Research shows that the majority of women aren’t receiving proper menopause-related healthcare. Even more concerning, common menopause symptoms are widely misunderstood and often brushed off by both patients and healthcare providers.
Why Are So Many Women Missing Out on Menopause Care?
The numbers are hard to ignore: between 3% and 75% of women remain untreated for menopause and perimenopause (0.00-0.05). That’s millions of women struggling in silence. Why does this happen? Part of the problem is that menopause symptoms are incredibly varied—there are more than 100 menopause-related symptoms, and most people (including doctors) overlook them (0.19). As one expert puts it:
“There’s more than 100 plus symptoms that women aren’t aware of.”
Think about that for a moment. Over 100 different ways your body might be telling you something is off with your hormone balance, yet so many of these signs are dismissed or misdiagnosed.
Common, Yet Overlooked, Menopause Symptoms
- Increased stress and anxiety (0.07-0.09)
- Unexpected weight gain, especially around the belly (0.09-0.12)
- Loss of libido and intimacy struggles (0.16-0.19)
- Brain fog and memory lapses
- Sleep disturbances
- Mood swings
- Hot flashes and night sweats
Many women, like my friend, have mistaken brain fog for early dementia, only to discover later that it was actually a hormone imbalance. This is more common than you might think. The lack of awareness around menopause symptoms means that women often accept these issues as just “part of aging,” missing out on real solutions that could dramatically improve their quality of life.
Why Do Women Accept This as Inevitable?
Society has a way of normalizing suffering, especially when it comes to women’s health. From a young age, you might have been told that discomfort, fatigue, or mood swings are just things you have to live with. Mainstream medicine often chalks up menopause symptoms to aging, rather than exploring hormone balance as a root cause (0.14-0.16). This messaging is so pervasive that many women don’t even realize there are more than 100 menopause symptoms—let alone that many of them are avoidable with the right approach.
Dr. Sarah Zal, a leading voice in women’s wellness, emphasizes that hormone health is foundational. She argues that with the right information and support, women can take charge of their wellness journey and address the root causes of their symptoms.
What’s Missing from Mainstream Care?
- Recognition of the full spectrum of menopause symptoms
- Personalized approaches to hormone balance
- Validation of women’s experiences, rather than dismissal
- Education about the options available for symptom relief
Studies indicate that when women are empowered with knowledge about menopause symptoms and hormone balance, they’re better equipped to advocate for their health. Yet, the gap between what women need and what they receive remains wide. The result? Too many women are left feeling isolated, frustrated, and resigned to symptoms that could be managed or even prevented.
If you’ve ever wondered why your usual stress management techniques aren’t working, or why your body feels unfamiliar, you’re not alone (0.07-0.14). The truth is, menopause and perimenopause are complex, and the care you deserve is often missing from the conversation. It’s time to rethink what’s possible for women’s wellness—and to demand better.
Section 2: Why Hormones Are More Like Text Messages Than a Bad Boss (Chart Inside)
When you think about hormones, you might imagine them as strict bosses, barking orders and controlling every move your body makes. But that’s not really how it works. In reality, hormones are more like text messages—quick, targeted, and surprisingly nuanced. They’re the internal DMs that keep your body’s systems in sync, sending vital instructions to organs, tissues, and even your brain, all day long (0.39-0.41).
Dr. Sarasal, a Harvard-trained physician and hormone expert, puts it simply: “Most people have imbalanced hormones…around 90% of them have a problem with their cortisol hormones.” (0.44-0.48) That’s not a typo. Out of the 40,000 patients Dr. Zal has tested and treated, an overwhelming 90% showed signs of cortisol hormone imbalance. This isn’t just a minor blip on your health radar. Research shows that hormone imbalance—especially involving cortisol—can have deep, lasting effects on your mental, physical, and metabolic health.
What Exactly Are Hormones Doing?
Hormones act as messengers within your body. They regulate everything from your energy levels to your mood, metabolism, and even how your body handles stress. Think of them as the group chat that never sleeps—one you can’t mute, even if you wanted to. When those messages get garbled or sent at the wrong time, things can go sideways fast.
Cortisol: The Stress Messenger
Let’s zero in on cortisol, often called the “stress hormone.” It’s supposed to help your body respond to challenges, but when cortisol levels stay high for too long, the effects can be damaging. According to Dr. Zal’s findings, excess cortisol is the most common hormone imbalance he sees (0.44-0.48). The effects? They’re more serious than you might think:
- More belly fat: High cortisol is linked to increased abdominal fat, which is harder to lose and riskier for your health (0.51-0.52).
- Brain shrinkage in women: Studies indicate that excess cortisol can actually shrink the brain in women—but not in men (0.54-0.57).
- Higher risk of depression: Elevated cortisol is associated with a greater risk of depression, making stress and hormones a key mental health concern (0.57-0.58).
- Lower testosterone: If your body is busy making too much cortisol, it makes less testosterone. This isn’t just a men’s health issue—women need testosterone too, and low levels can trigger a cascade of problems (1.00-1.03).
How Do You Know If You Have a Hormone Imbalance?
You might have heard that hormone levels are mysterious or hard to measure. That’s not true. Hormone imbalances, including cortisol effects, are measurable via simple blood tests. These tests can reveal the root causes behind symptoms like fatigue, weight gain, mood swings, and more. If you’ve ever wondered why you feel “off” even when your basic labs look normal, it might be time to check your hormones.
Imagine Reading Your Body’s Group Chat
Here’s a wild thought: What if you could read every message your body sends itself? Would you ever ignore those notifications? Probably not. Yet most people walk around completely unaware of the internal conversations happening every second. Understanding your hormone signals is like unlocking a whole new level of self-awareness—and it can be the key to better health.
Most people have imbalanced hormones…around 90% of them have a problem with their cortisol hormones.
Chart: Hormone Imbalances in Dr. Zal’s Patients
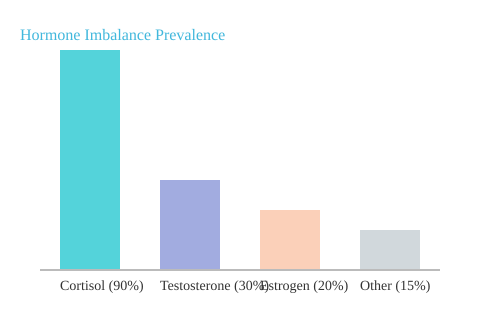
The chart above illustrates just how common hormone imbalances are, especially when it comes to cortisol. If you’re experiencing unexplained symptoms, don’t ignore your body’s messages. Understanding the effects of stress and hormones could be the missing piece in your health puzzle.
Section 3: When Childhood Trauma Haunts Your Body—The ACE Test and A Personal Detour (Table Inside)
Have you ever wondered how your childhood experiences might be shaping your health right now? It’s not just an abstract idea—research shows that adverse childhood experiences (or ACEs) are deeply connected to your risk for chronic diseases later in life (1.08-1.18). The ACE test, a simple yet powerful questionnaire, is one of the most validated ways to measure the impact of trauma and health over a lifetime. And the results can be, frankly, shocking.
What Is the ACE Test?
The ACE test stands for Adverse Childhood Experiences. Developed in the 1990s, it’s a set of 10 questions that ask about things like parental divorce, emotional or physical abuse, neglect, and having a parent with a substance use disorder (13.36-14.08). Each “yes” answer adds a point to your ACE score. The higher your score, the greater your risk for a wide range of health problems—sometimes decades after the events themselves.
How ACE Scores Predict Chronic Disease Risk
Here’s where it gets real: studies indicate that people with an ACE score of 1 or higher have a significantly increased risk of developing 45 different chronic diseases as adults (1.14-1.18). These aren’t just minor issues. We’re talking about heart disease, diabetes, autoimmune disorders, depression, and even certain cancers. As Dr. Zal puts it,
“People who had one or higher ACE scores had a greater risk of 45 different chronic diseases.”
That’s not just a statistic—it’s a wake-up call. Trauma isn’t just in your head. It’s literally embedded in your biology, shaping your immune system, hormones, and even your DNA.
Dr. Zal’s Personal Detour: Healing Without Pharmaceuticals
To make this even more relatable, Dr. Zal shares her own story. Her ACE score? Six out of ten (13.47-13.53). That’s high. She experienced parental divorce at age one, along with other forms of adversity. Instead of turning to pharmaceuticals, she used lifestyle medicine—nutrition, movement, stress reduction, and social connection—to restore her health and resilience. It’s a powerful reminder that knowing your ACE score isn’t about labeling yourself. It’s about understanding your risk and taking proactive steps to heal.
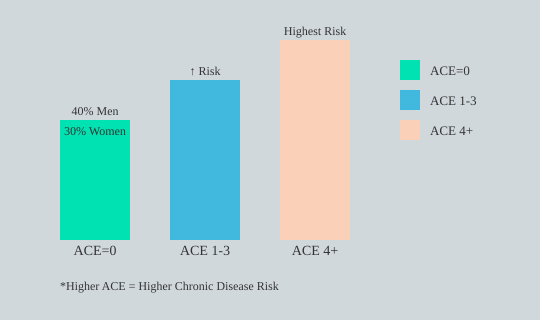
How Common Are High ACE Scores?
Not everyone has a high ACE score. In fact, about 40% of men and 30% of women have an ACE score of zero (Data). But that means the majority of us have at least one. And for those with higher scores, the risk for chronic disease climbs even more. What’s tricky is that symptoms may not show up until years—or even decades—later. You might develop “mystery” symptoms or chronic illnesses that seem to come out of nowhere, but are actually rooted in early life experiences (14.32-14.51).
Why Unpacking Your Story Matters
So, why should you care about your ACE score? Because understanding your own history can shape your prevention and healing strategies. Ignoring the past doesn’t make it disappear; it just buries it deeper in your biology. As research shows, unpacking your early stories can be the key to breaking cycles of illness and reclaiming your health as an adult (14.34-15.04).
ACE Scores and Chronic Disease Risk: The Data
Let’s break down the numbers visually. The chart below illustrates the relationship between ACE score categories and chronic disease risk, with a gender breakdown for ACE=0. It’s a stark reminder of how common adverse childhood experiences are—and how much they matter for your lifelong health.
Understanding your ACE score isn’t just about the past—it’s about empowering your future. Trauma and health are intertwined, but with knowledge comes the power to change your story.
Section 4: Beyond the White Coat—The Rise of the Doctor as Healer and Data Detective
When you think of a doctor, what comes to mind? Maybe a white coat, a prescription pad, and a quick diagnosis. But what if your doctor saw themselves as a healer first—a partner in unlocking your body’s own ability to recover? Dr. Sarah Zal is part of a new wave of physicians blending scientific rigor with a deep respect for your unique story, your data, and your innate resilience. This is the heart of precision medicine and the modern healer doctor—and it’s a far cry from the one-size-fits-all approach you might expect.
From Harvard-MIT to Healing Intuition
Dr. Zal’s journey is anything but typical. Her training started at the intersection of science and innovation, as a bioengineer in the Harvard-MIT program (2.46-3.54). This program is designed to create physician-scientists who push the boundaries of academic medicine. She went on to complete a residency in obstetrics and gynecology, then expanded her expertise to primary care—treating not just women, but men as well (3.39-4.52).
But here’s where it gets interesting. Despite her mainstream medical background, Dr. Zal describes herself as a healer (2.23-2.26). What does that mean? She explains, “It means that my task is to connect to your innate healing capacity and to work with you to activate it” (2.32-2.44). In her view, healing isn’t something she does to you. Instead, she works with you—helping you identify and remove obstacles so your body can do what it’s designed to do.
“What I do is I work with someone who’s got the capacity to heal and we work to be in the service of that.” (3.10-3.21)
Precision Medicine: Your Unique Blueprint
Traditional medicine often treats you as an “average patient.” But precision medicine is different. It’s about understanding your unique biology, history, and even your life story. Dr. Zal’s approach is grounded in the belief that real healing requires both data and intuition. She’s treated over 40,000 patients, harnessing big data to spot patterns and personalize care (5.18-5.19). But she also draws from ancient wisdom—Ayurveda from India, Traditional Chinese Medicine, and other holistic traditions (4.18-4.33).
Research shows that true healing takes scientific rigor blended with a respect for the patient’s innate resilience. This is where Dr. Zal’s dual expertise shines. She’s as comfortable crunching numbers as she is listening deeply to a patient’s narrative. Her role as Director of Precision Medicine at the Marcus Institute in Philadelphia is proof that this model isn’t just theoretical—it’s being put into practice at the highest levels.
Moving Beyond the Pill: The Healer Doctor in Action
Ever had a doctor say, “Let’s unblock your own healing,” instead of just handing you a prescription? Dr. Zal’s patients include professional athletes, executives, and everyday people (2.44-2.54). Her method is collaborative, not paternalistic. She doesn’t see herself as the hero swooping in to fix you. Instead, she helps you understand what’s getting in the way of your best health and how to move past it (3.23-3.37).
Studies indicate that personalized care—the cornerstone of precision medicine—represents a significant departure from “average-based” care. It’s about crafting individualized health plans based on your data, your goals, and your lived experience. Dr. Zal’s mosaic career—spanning surgery, data science, and deep patient listening—shows what’s possible when medicine is both an art and a science.
- Academic rigor meets healing intuition
- Big data and ancient wisdom, side by side
- Each patient’s story is central, not secondary
In the end, the modern healer doctor is a data detective, a guide, and a collaborator. Precision medicine isn’t just a buzzword—it’s a promise that your care will be as unique as you are.
Section 5: Food, Breathwork, and Breaking the Myth of ‘Just Take the Pill’ (Chart Inside)
When you walk into most doctor’s offices, you might expect a prescription pad to come out before you’ve even finished describing your symptoms. But Dr. Zal’s approach flips this script entirely. Instead of reaching for a quick-fix pill, he starts with the basics: lifestyle medicine, personalized nutrition, and prevention. As he puts it, “Getting their hormones back into balance…starting first with lifestyle medicine, not a pharmaceutical” (5.13-5.20).
Why Lifestyle Medicine Comes First
Dr. Zal sees hormones as the entry point for most people seeking his help. But rather than defaulting to medication, he emphasizes the power of lifestyle tweaks—especially breathwork and nutrition. These aren’t just buzzwords. They’re foundational tools that can dramatically shift your health, especially when tailored to your unique needs (5.36-6.15).
- Breathwork: Often overlooked, breathwork is one of the most underutilized tools in health. Regular practice can help balance hormones, support mitochondrial function, and boost daily energy (6.17-6.27).
- Nutrition: Forget generic meal plans. Dr. Zal focuses on what’s optimal for you—your genetics, your job, your life stage. Whether you’re a professional athlete, a podcaster, or a parent juggling a million things, your nutrition plan should reflect your reality (6.30-7.12).
- Prevention: Prevention isn’t glamorous, but it’s essential. Dr. Zal notes that lifestyle medicine could prevent or reverse at least 70% of chronic diseases. Yet, as he says, “Prevention has been a hard thing to sell” (7.18-7.27).
Personalized Nutrition: No More One-Size-Fits-All
Have you ever been given dietary advice by someone who never asked about your routines, cravings, or even your goals? It’s frustrating—and often ineffective. Dr. Zal’s approach is different. He believes nutrition advice should be as unique as you are. Research shows that personalized nutrition, based on your genetics, occupation, and life stage, is far more effective than generic recommendations. This is where lifestyle medicine shines: it’s about finding what works for you, not just what works for the average person.
Chronic Illness Prevention: The Untapped Potential
Imagine if we treated pre-diabetes with the same urgency as a common cold. How many lives—and healthcare dollars—could we save? Studies indicate that up to 70% of current diseases are preventable through lifestyle medicine. Yet, prevention often lacks the “sex appeal” of a new drug or trendy supplement. Dr. Zal works with people across the health spectrum, from those in a state of health to those teetering on the edge of chronic disease, like pre-diabetes. Early intervention, he says, is key to reversing disease before it takes hold (7.34-7.56).
Lifestyle medicine prevents 70% of [chronic disease].
Personalization Is Key—For Everyone
Whether you’re an entrepreneur, a professional athlete, or “just” a busy parent, a one-size-fits-all solution simply doesn’t cut it. Dr. Zal’s work is rooted in the belief that individualization is essential. He takes into account your genetics, your goals, and your current life stage to craft a plan that fits you—not the other way around. This isn’t just theory; research supports that personalized lifestyle interventions could prevent most chronic disease, saving both lives and costs.
Table: The Power of Lifestyle Medicine
| Key Area | Impact | Personalization Factor |
|---|---|---|
| Chronic Disease Prevention | Up to 70% preventable via lifestyle medicine | Tailored to individual risk factors |
| Nutrition | Improved metabolic health and energy | Based on genetics, occupation, and goals |
| Pre-diabetes & Metabolic Health | Early intervention can reverse disease | Requires ongoing, personalized monitoring |
So, next time you’re offered a quick prescription, pause and ask: is there a lifestyle tweak that could work better for me? Personalized nutrition and lifestyle medicine might just be the missing piece in your journey toward lasting health.
Section 6: If Medicine Is Broken, How Do We Fix It? The Precision Revolution
If you’ve ever felt like your medical care is designed for “the average person,” you’re not alone. Modern healthcare, especially for chronic illness prevention, often relies on a one-size-fits-all approach. But you deserve more than average results. Let’s look at why the system is failing—and how the rise of precision medicine could change everything (8.34–8.39).
Medicine for the Average: Why Mainstream Care Falls Short
Mainstream medicine is built around treating large groups with the same solution. For example, if you have high cholesterol, you’re likely prescribed a statin. But here’s the catch: research shows that to help just one person, doctors need to treat 100 to 200 people with statins (9.09–9.13). As one expert put it:
“We have to treat about 100 to 200 people for one person to benefit.”
That means most people are exposed to the risks and costs of medication without seeing any real benefit. This is what some call “imprecision medicine”—treating everyone the same, regardless of their unique biology or life circumstances (8.39–8.47).
Why Pharmaceuticals Dominate—and Lifestyle Gets Ignored
You might wonder why the focus is so heavy on drugs like statins or GLP1s. The answer is simple: profit. Randomized controlled trials, considered the “gold standard” in medicine, are usually designed around pharmaceuticals, not lifestyle changes (10.05–10.16). There’s little financial incentive to promote lifestyle medicine, even though research indicates that 70% of chronic diseases are preventable through changes in diet, exercise, and stress management (10.49–10.54).
So, while lifestyle medicine could help the majority, it’s often sidelined. Instead, the system leans on drugs—solutions that are more lucrative for the industry but less effective for you as an individual.
Precision Medicine: Personalized Care for Real Results
This is where precision medicine comes in. Instead of treating you like just another number, precision medicine digs deep. It uses your genomics, biomarkers, wearable data, and even your own health experiments (called N-of-1 or NF1 studies) to tailor care specifically to you (9.19–9.44).
- Genomics: Your unique DNA can reveal risks and guide prevention strategies.
- Biomarkers: Regular bloodwork and other tests show how your body is functioning in real time.
- Wearables: Devices track your sleep, activity, and heart rate, providing actionable data.
- N-of-1 Experiments: You become your own case study, testing what works best for your body and goals.
In this model, you’re not just a patient—you’re the experiment, the data, and the decision-maker. Your story, your preferences, and your results shape your care plan (9.42–9.47).
Reimagining Chronic Disease Prevention
Imagine a system where your care isn’t dictated by what works for “most people,” but by what works for you. Precision medicine means using all available data—your genetics, your lifestyle, your preferences—to guide every intervention. This approach is especially powerful for chronic illness prevention, where small, personalized changes can make a huge difference.
Studies indicate that mass medicine is less effective than tailored, precision-based approaches. Yet, because lifestyle medicine isn’t as profitable, it’s often ignored. It’s time to shift the focus from profit-driven care to truly personalized care—where prevention and individual needs come first.
| Approach | Key Data |
|---|---|
| Statin Treatment | Treating 100–200 people = 1 person benefits |
| Lifestyle Medicine | 70% of chronic diseases preventable |
| Precision Medicine | Uses genomics, biomarkers, and NF1 (N-of-1) experiments |
The revolution in medicine is here. It’s about moving beyond “average” and making care truly personal—because you’re not average, and your health shouldn’t be either.
Section 7: FAQs—Let’s Get Real About Hormones, Trauma, and Healing
Let’s cut through the noise and get practical about hormone balance, trauma and health, and the promise of lifestyle medicine. If you’ve made it this far, you’re likely hungry for clear, actionable answers. Dr. Sarah Zal’s insights, drawn from decades of experience and thousands of patients, offer a refreshing dose of reality—so let’s tackle the questions you’re probably asking yourself.
Can I Really Measure and Fix My Hormones?
Absolutely—you can measure your hormones, and you can take steps to improve them. Dr. Zal emphasizes that most people, even high performers, have some degree of hormonal imbalance, with cortisol being the most common culprit. Testing isn’t just for elite athletes or celebrities. You can start with basic bloodwork (think cortisol, insulin, thyroid, estrogen, testosterone, and vitamin D), and even leverage wearables and continuous glucose monitors for real-time feedback. The key is to use these tools as guides, not as a one-time fix. Research shows that tracking your biomarkers and making small, consistent lifestyle changes—like improving sleep, managing stress, and eating more fiber—can have a profound impact on hormone balance.
What’s a Realistic First Step if I Suspect My Symptoms Are Hormone-Related?
If you’re experiencing unexplained fatigue, mood swings, belly fat, or sleep issues, don’t panic. The first step is awareness. Start by tracking your symptoms and daily habits. Next, ask your doctor for a basic hormone panel. If your provider isn’t receptive, consider seeking out a specialist in lifestyle medicine or precision medicine. As Dr. Zal points out, the system is often slow to catch up, so being your own advocate is essential. Even small shifts—like prioritizing sleep, reducing processed foods, and practicing stress management—can start to move the needle.
How Much Does My Childhood Impact My Health?
More than most people realize. The science around trauma and health is compelling. The ACE (Adverse Childhood Experiences) test is a simple, ten-question tool that predicts risk for 45 chronic diseases. Even a score of 1 raises your risk. Dr. Zal’s own ACE score is 6, and she’s candid about how trauma can show up as depression, pre-diabetes, or hormone issues later in life. But here’s the good news: understanding your history gives you power. Addressing trauma—through therapy, lifestyle medicine, or even practices like breathwork—can help you break the cycle and reclaim your health.
Who Should Consider Precision Medicine?
Precision medicine isn’t just for people with rare diseases or those who want to optimize athletic performance. It’s for anyone who wants to move beyond “average” care and get answers tailored to their unique biology. If you’ve struggled with chronic symptoms, have a family history of disease, or simply want to feel your best, precision medicine offers a roadmap. Dr. Zal’s approach—using genomics, wearables, and real-time data—helps you understand what works for your body, not just what works for most people.
Is Breathwork Actually Legit, or Just a Wellness Fad?
Breathwork is more than a fleeting trend. Studies indicate that practices like resonance breathing (for example, a 5-second inhale and 7-second exhale) can lower cortisol, improve heart rate variability, and support hormone balance. Dr. Zal uses these techniques with her patients, from stressed executives to athletes, because they work. The beauty of breathwork is its accessibility—you don’t need fancy equipment, just a few minutes and a willingness to try.
Why Isn’t My Doctor Talking to Me About Any of This?
This is a question Dr. Zal hears all the time. The reality is, most medical training still focuses on pharmaceuticals and acute care, not prevention or lifestyle medicine. Dr. Zal herself received only 30 minutes of nutrition and menopause education in medical school. The system is slowly changing, but you may need to seek out providers who specialize in hormone balance, trauma and health, or lifestyle medicine. In the meantime, don’t be afraid to ask questions, request testing, and take charge of your own health journey.
In the end, your path to healing is personal. Whether you’re grappling with hormone imbalances, the legacy of trauma, or just want to feel better, the most important step is to start. Use science, trust your instincts, and remember: you are your own best advocate. As Dr. Zal’s story shows, transformation is possible—one informed, intentional step at a time.
TL;DR: You are not destined for fatigue, belly fat, or stress just because ‘that’s life’ or you’re getting older. Focusing on hormone balance, understanding your unique history (yes, even your childhood), and demanding better, personalized care could be your ticket to feeling alive again. Don’t settle: the science and lived experience are finally aligning in your favor.
Hats off to The Diary Of A CEO for the incredibly insightful content. Be sure to take a look here: https://youtu.be/0GQozcTPyO0?si=ML0hgtgBxOHAqXtb.