Let me start with a confession. Until last year, I’d never heard of ‘sexspan’ either. Then a friend playfully tossed out the term at a dinner party, sparking a debate that got awkward, honest, and—dare I say—more educational than my high school health class. Why do we silently assume our sex lives will just keep working until our bodies don’t? Why is it so hard to ask for help? Turns out, there are answers—many of them, in fact: scientific, practical, and sometimes just delightfully weird.
The Mystery and Science Behind Sexspan: What Is It, and Why Does It Matter?
Let’s talk about something that’s rarely discussed openly, but affects nearly everyone: sexspan. If you haven’t heard the term before, you’re not alone. The sexspan definition is simple—sexspan means the length of time you can enjoy satisfying sexual activity during your life. While most people hope their sexspan will match their lifespan, the reality is often quite different.
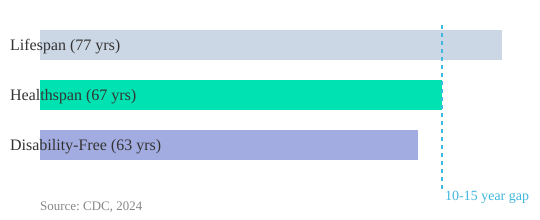
To understand why, let’s look at the numbers. According to the CDC, the average lifespan in the United States is 77 years (2.59-3.02). But here’s where things get interesting: your health span—the years you live in good health—is only about 67 years (3.05-3.09). And if you dig deeper, the average American will spend just 63 years without any disability (3.11-3.16). That leaves a gap of 10 to 15 years, sometimes more, where chronic health issues, disability, or untreated conditions can impact not just your daily life, but your ability to enjoy intimacy (3.16-3.22).
Why the Gap Between Lifespan, Health Span, and Sexspan Matters
So, what does this mean for your sex life? Research shows that sexspan—the period in which you can participate in satisfying sexual activity—often ends before your healthspan, and well before your actual lifespan. This gap isn’t just a number; it’s a real quality-of-life issue. Many people find themselves struggling with intimacy, desire, or physical ability years before they expected. Sometimes it’s due to chronic health problems, sometimes it’s hormonal changes, and sometimes it’s relationship factors. But the result is the same: a loss of something deeply connected to happiness and wellbeing.
As one sexual medicine expert puts it:
“Sexspan is the ability to engage in satisfying sexual activity, and you want that to last as long as possible.”
It’s a simple statement, but it cuts to the heart of the matter. Sexual wellbeing isn’t just about pleasure—it’s tied to your mental, physical, and emotional health. Studies indicate that people who maintain an active and satisfying sex life often report greater happiness, stronger relationships, and even better physical health. Yet, despite its importance, we rarely talk about how to protect or extend our sexspan until problems arise.
Sexual Health: More Than Just Libido
When you think about sexual health tips, you might picture advice about boosting libido or spicing up your relationship. But the science goes deeper. Research shows that talking and planning for sexual health earlier in life can actually extend your sexspan. Open conversations with your partner and healthcare provider, lifestyle changes like exercise and nutrition, and addressing chronic health issues proactively all play a role.
Here’s what the data tells us:
- Average U.S. lifespan: 77 years
- Average health span: 67 years
- Disability-free years: 63 years
- Sexspan often ends 10-15 years before lifespan
That’s a significant chunk of time where intimacy could be lost—unless you take steps to protect it. The good news? Science suggests there are actionable ways to extend your sexspan, from managing chronic conditions to maintaining open dialogue about your needs and desires.
Why Don’t We Talk About Sexspan Sooner?
Despite its impact, sexspan is a topic that’s only recently gained attention among sexual medicine experts. Maybe it’s because talking about sex and aging still feels taboo. Or maybe it’s because many people assume that a decline in sexual wellbeing is just a normal part of getting older. But it doesn’t have to be. By understanding the science and embracing honest conversations, you can take control of your sexual health—and potentially enjoy a longer, more satisfying sexspan.
Understanding your sexspan—and how it fits into your overall health span—can empower you to make choices that support your wellbeing for years to come. The science is clear: with the right knowledge and proactive steps, your sexspan can last longer than you might think.
Four Pillars for Supercharging Your Sexspan (and Why There’s No Magic Pill)
When it comes to extending your sexspan—that is, the number of years you can enjoy healthy sexual function—there’s a lot of noise out there. You’ve probably seen ads promising a quick fix or a miracle supplement. But if you look at what the science actually says, the real answers are much simpler and, honestly, a bit less glamorous. The four pillars that matter most are diet, exercise, sleep, and stress reduction (3.48-3.51). If you’re looking for sexual health tips that actually work, these are the places to start.
Let’s break down why these pillars are so powerful, and why there’s truly no magic pill that can replace them.
Diet: The Foundation for Libido and Hormonal Health
Your diet doesn’t just affect your waistline—it has a direct impact on your libido and overall sexual function. Research shows that obesity is a leading driver of low testosterone and sexual dysfunction in both men and women. Processed foods, excess sugar, and unhealthy fats can disrupt your hormones, sap your energy, and leave you feeling less interested in sex. On the flip side, simple changes like eating more whole foods, lean proteins, and healthy fats can help improve sexual function and support your body’s natural hormone production.
Exercise: Boost Testosterone and Sexual Vitality
Physical activity is one of the most effective ways to improve sexual function and boost your libido. Regular exercise helps regulate hormones, increase blood flow, and reduce stress—all of which are essential for a healthy sex life. Studies indicate that even moderate activity, like brisk walking or cycling, can have a positive testosterone impact and enhance your mood. You don’t need to become a gym fanatic; just moving more each day can make a noticeable difference.
Sleep: The Most Overlooked Pillar
Of all the pillars, sleep is often the hardest to prioritize—and the most underestimated. Lack of sleep is a silent saboteur of sexual health. Research shows that poor sleep quality can lower testosterone levels, increase stress hormones, and reduce your interest in sex. If you’re struggling with low libido or sexual dysfunction, improving your sleep habits might be the most powerful change you can make. Try setting a consistent bedtime, limiting screens before bed, and creating a restful environment. It’s not glamorous, but it works.
Stress Reduction: The Unsung Hero for Libido
Chronic stress is a major libido killer. It disrupts your hormones, increases inflammation, and makes it hard to relax and enjoy intimacy. Simple stress-reduction techniques—like mindfulness, deep breathing, or even just taking a walk—can help restore hormonal balance and improve your overall sense of well-being. Remember, lifestyle for libido isn’t just about what you do in the bedroom; it’s about how you manage your mind and body every day.
‘I don’t have a pill on the planet stronger than diet, exercise, sleep, and stress reduction.’ (3.51-3.59)
Why There’s No Shortcut—And Why That’s Good News
It’s tempting to look for a quick fix, especially when you’re frustrated by low libido or sexual health challenges. But the truth is, no supplement or medication can match the power of these four pillars. Testosterone replacement therapy can help some people, but it’s not a panacea—especially for women. The real secret to extending your sexspan is in the small, daily choices you make. Walking more, cutting out processed foods, getting enough sleep, and managing stress will do more to improve sexual function than any pill on the market.
Experts agree: there’s simply no substitute for good habits when it comes to sexual wellness. If you want lasting results, focus on these four pillars. They’re not always easy, but they’re always worth it.
Numbers Nobody Talks About: Sexual Dysfunction by the Stats (And What They Mean for You)
When you think about sexual health, you might imagine it’s a private issue—something that only affects a few people, or something that’s “just part of getting older.” But the reality is far different. The numbers around sexual dysfunction are not only staggering, they’re also rarely discussed openly. If you’re looking for real sexual dysfunction awareness, it starts with understanding the facts and what they mean for your health and relationships.
Female Sexual Dysfunction: The Silent Struggle
Let’s start with women. Research shows that in the United States, about 43-48% of women experience female sexual dysfunction (FSD) (see transcript 0.35-0.38). That’s nearly half of all women, yet the topic is often brushed aside or treated as taboo. FSD isn’t just about low libido—it includes issues with desire, arousal, orgasm, and pain during sex. These are real, measurable problems that can impact emotional wellbeing, self-esteem, and even relationships.
Despite how common it is, female sexual dysfunction is still underdiscussed—even among healthcare professionals. Many women don’t realize how prevalent it is, or that there are effective treatments available. This lack of sexual dysfunction awareness can leave you feeling isolated, when in fact, you’re far from alone.
Erectile Dysfunction Stats: More Than Just a Bedroom Issue
For men, the numbers are just as striking. Premature ejaculation affects 30% of men worldwide (0.44-0.47). And by the age of 40, 40% of men will experience erectile dysfunction (ED) (0.47-0.49). These erectile dysfunction stats aren’t just about performance—they’re about health.
Here’s where things get even more serious: “Erectile dysfunction is the first sign of other major adverse medical problems.” (0.51-0.53) Studies indicate that ED can be an early warning sign for underlying conditions like heart disease and depression. In fact, 66% of men with ED also experience some degree of depression (0.55-0.58). Even more alarming, 15% of men with ED will have a heart attack or stroke within seven years of diagnosis.
“Erectile dysfunction is the first sign of other major adverse medical problems.”
Why Sexual Dysfunction Signals Bigger Health Risks
Sexual dysfunction isn’t just a quality-of-life issue—it’s a leading indicator of other health risks. If you or your partner are experiencing symptoms, it’s not just about sex. It’s about your overall health. Research shows that addressing sexual dysfunction early can help uncover and manage serious problems like cardiovascular disease or depression.
Unfortunately, most primary care doctors receive limited education in sexual health (training gaps). This means many cases go undiagnosed or untreated, leaving patients to struggle in silence. The stigma around sexual dysfunction only makes this worse. People are often too embarrassed to bring it up, and doctors may not ask.
Sexual Dysfunction Awareness: Why Openness Matters
Both men and women face high rates of sexual dysfunction, yet rarely is it treated with the seriousness or openness it deserves. The data is striking—and sobering. But here’s the good news: sexual dysfunction is common and treatable. Greater openness in discussing and addressing sexual health improves outcomes for everyone involved.
If you’re struggling, know that you’re not alone. These numbers aren’t just statistics—they’re real people, real relationships, and real opportunities for better health. The first step is awareness. The next is honest conversation—with yourself, your partner, and your healthcare provider.
Sexual Dysfunction: Prevalence & Health Risks
43-48% of US women (FSD)
30% of men (PE)
40% of men at 40 (ED)
66% of men with ED (depression)
15% of men with ED (heart attack/stroke in 7 yrs)
FSD
PE
ED@40
Depression
Cardiac
Courage to Ask (Even if You’re Blushing): The Power of Sexual Health Conversations
Let’s be honest—sexual health communication is one of the most avoided topics in both clinics and bedrooms. Even when sex is directly impacting your health or relationship, it’s common to keep quiet. Why? Shame, embarrassment, and the simple fact that most doctors aren’t well-trained to ask the right questions. As a result, you might feel alone with your concerns, unsure where to turn or how to start the conversation (7.10-7.11).
Research shows that this silence can prolong problems needlessly. When you avoid talking about sexual issues, you’re not just dodging discomfort—you’re also missing out on solutions that could make a real difference. Honest conversations, whether with your partner or healthcare provider, are often the fastest route to relief and better intimacy.
Why Doctors (and Patients) Struggle to Talk About Sex
It’s not just you. Most people—patients and doctors alike—find it difficult to bring up sexual health. According to studies, only 65% of US medical students receive any training in sexual medicine. Of those, half rate their training as “terrible” (7.27-7.35). That means many doctors feel just as awkward or unprepared as you do.
| Statistic | Value |
|---|---|
| US medical students receiving sexual medicine training | 65% |
| Of those, rating training as ‘terrible’ | 50% |
| Depression comorbid with ED | 66% |
| Performance anxiety as an underdiagnosed cause | Common |
Doctors rarely screen for erectile dysfunction (ED), female sexual dysfunction (FSD), or libido problems during routine visits (7.20-7.27). So, if you’re waiting for your provider to bring it up, you might be waiting a long time.
Different Words, Different Worlds: Men and Women Speak Differently About Sex
Men and women often describe their sexual concerns in very different ways (7.11-7.14). Personal language nuances can cloud understanding, even between partners. For example, men might focus on physical function, while women may talk about desire or emotional connection. These differences can make it harder to pinpoint the real issue—unless you’re willing to ask direct questions.
Simple Questions, Powerful Answers
When it comes to diagnosing sexual dysfunction, a few straightforward questions can reveal a lot. For men, two simple yes/no questions are often enough (7.53-8.03):
- Are you able to get an erection sufficient for penetration?
- Are you able to maintain that erection to orgasm or pleasure?
If the answer to either is “no,” that’s a clear sign of erectile dysfunction. These questions cut through embarrassment and get right to the heart of the matter.
The Hidden Role of Psychology
It’s not always about physical health. Psychological components—like performance anxiety or depression—often lurk beneath the surface (7.39-8.16). In fact, research indicates that 66% of men who come in with ED have some degree of depression. As one expert puts it:
You have to query about depression because 66% of men who come in with ED have some degree of depression.
Performance anxiety is another underdiagnosed cause of sexual dysfunction. If you’re struggling, you’re not alone—and you’re not “broken.” Sometimes, talking about your worries is the first step toward improvement.
Why Honest Conversations Matter for Couples Intimacy
Talking honestly about sexual issues—whether in the clinic or at home—is nearly always the missing link to improvement. Yet shame and stigma keep many from starting the conversation. Sex therapy and open sexual health communication can help you and your partner understand each other better, break down barriers, and find solutions together.
If you’re unsure where to start, remember: a simple, direct question can open the door to better couples intimacy and a healthier sex life. Don’t let embarrassment keep you from the help—and happiness—you deserve.
When Your Heart and Your Libido Are Talking: Links Between Sex, Cardiovascular, and Mental Health
When you think about erectile dysfunction (ED), you might picture it as a private, bedroom-only concern. But research shows that ED is often much more than a sexual health issue—it’s a potential early warning sign for serious cardiovascular problems. In fact, the link between your heart, your libido, and your mental health is stronger than most people realize. Understanding these connections could be lifesaving, not just life-changing.
Erectile Dysfunction: More Than Just a Bedroom Issue
Let’s start with some eye-opening erectile dysfunction stats. Studies indicate that about 15% of men diagnosed with ED will experience a heart attack or stroke within seven years (9.28-9.36). That’s not a small number. When you come in with ED, you’re not just talking about sex—you could be talking about your heart’s future. As one expert puts it,
“Erectile dysfunction is the first sign of other major adverse medical problems.”
But why does ED show up before other cardiac symptoms? The answer lies in the size of your arteries. The arteries supplying blood to the penis are only about 1 to 2 millimeters wide, while coronary arteries are 3 to 4 millimeters, and carotid arteries are even larger (9.54-10.06). If plaque is building up in your arteries, the smallest ones get blocked first. That means ED can appear years before you ever feel chest pain or have a cardiac event (arterial diameter theory).
ED as a Predictor: The Timeline Matters
One of the most striking findings comes from research showing that, on average, there’s a 39-month gap between the onset of ED and a cardiac emergency like a heart attack (9.47-9.50). That’s over three years—a window of opportunity for you and your doctor to intervene, manage risk factors, and potentially prevent a life-threatening event. Another study from Greece found that 1 in 5 men with ED had significant blockages in their heart vessels even before any heart symptoms appeared.
| Key Statistic | Value |
|---|---|
| Heart attack/stroke after ED diagnosis | 15% (in 7 years) |
| Average time from ED onset to cardiac emergency | 39 months |
| Men with ED and blocked arteries (Greek study) | 20% (1 in 5) |
| Anxiety prevalence with ED | 35% |
Cardiac Risk, Sex, and the Overlooked Role of Mental Health
It’s not just about your arteries. Mental health and libido are deeply intertwined. Anxiety and depression are tightly linked to poor sexual function, but these issues are often missed during clinic visits. Research shows that 35% of men with ED also struggle with anxiety, and up to 66% experience depression. These mental health concerns can both cause and result from sexual dysfunction, creating a cycle that’s hard to break without honest conversations and proper screening.
Why does this matter? Because screening for ED (and asking about libido) could save lives, not just marriages. When you bring up changes in your sexual health, you’re giving your doctor a chance to look deeper—at your heart, your mental health, and your overall well-being. Sometimes, a check-up for libido leads to a much bigger medical discovery.
Knowledge Is Power: Don’t Ignore the Overlap
Many people aren’t aware of these medical overlaps. ED doesn’t just affect your sex life; it can be a crucial clue about your cardiovascular and mental health. If you notice changes in your sexual function, don’t brush them off. Instead, see them as a signal—one that’s worth discussing openly with your healthcare provider.
By understanding the links between erectile dysfunction stats, cardiac risk sex, and mental health and libido, you empower yourself to take charge of your health in ways that go far beyond the bedroom. Sometimes, the most personal symptoms are the ones that matter most for your whole-body wellness.
Libido Wars: Why Couples (Almost) Never Lose It at the Same Time
When it comes to libido problems in relationships, one of the most surprising truths is that couples almost never experience changes in desire at the same time. If you’ve ever wondered why your partner’s sex drive seems out of sync with yours—or why “fixing” one person’s libido doesn’t always fix the relationship—you’re not alone. The science and stories behind couples intimacy reveal just how complex this issue really is.
Libido: More Than Just a Mood
Libido isn’t just about wanting sex. It’s a complicated mix of hormones, brain chemicals, relationship dynamics, and even life stress. Research shows that hormonal status, mental health, and the quality of your connection with your partner all play a role. So, when one partner suddenly has more (or less) interest in sex, it’s rarely just about attraction or willpower. It’s biology, psychology, and partnership all tangled together.
The “PET” Hormones: Your Libido’s Secret Drivers
Doctors and therapists often use the acronym PET—Prolactin, Estrogen, Thyroid, and Testosterone—to guide their work-ups for hormone therapy sexuality concerns. These four hormones are the main players in sexual desire for both men and women:
- Prolactin: High levels can lower libido, especially after orgasm or with certain medications.
- Estrogen: Essential for arousal and lubrication, especially in women.
- Thyroid: Both overactive and underactive thyroids can cause libido problems.
- Testosterone: The classic “sex hormone,” but important for all genders.
Remember, antidepressants can also lower libido by raising serotonin, which is why medication side effects often show up in the bedroom.
Why “Fixing” One Partner Can Break the Couple
Here’s where things get tricky. Imagine a scenario straight from the clinic: A man is treated for erectile dysfunction and suddenly has a strong libido and great erections. But his wife isn’t ready for this new energy. In fact, she’s upset—her desire hasn’t changed, and now she feels pressured (see transcript 6.08-6.21). She calls the doctor, furious: “You’re treating my husband, you’re able to get him these great erections, great libido, but I don’t want to have sex with him and he wants to have sex with me all the time and now we have a terrible relationship. You’ve ruined our relationship!”
This isn’t just an anecdote—it’s a pattern. As one expert puts it:
“In sexual medicine, either both partners need a libido boost, or you’re setting up for disaster.”
When only one person’s sexual health is addressed, the couple can end up more out of sync than ever. That’s why a couple-centered approach is vital when treating sexual dysfunction or low libido. Medication and hormone imbalances often impact both partners differently, and treating just one side of the equation can actually make things worse.
Sexspan: A Couples’ Project, Not an Individual One
Think of your sex life as a shared project—a “sexspan” that you build and maintain together. It’s common for one partner to feel “fixed” while the other is still struggling. This mismatch can strain even the strongest relationships. Sex therapists recommend ongoing, honest conversations and joint solutions to these mismatches. Regular check-ins can help both partners stay in sync, even when desire naturally ebbs and flows.
It’s also important to note that testosterone therapy options for women remain limited compared to men, which can make treating female libido problems more challenging. That’s why understanding the medical and emotional roots of libido mismatches is so important. When both partners are involved in the process, outcomes are better for everyone.
When Intimacy Feels Like a Battlefield
Libido mismatches often strain relationships, but they don’t have to spell disaster. By recognizing that desire is influenced by hormones, mental health, and relationship quality, you can approach couples intimacy with more empathy—and better results. Honest conversations, medical check-ups, and a willingness to work together are the real secrets to extending your sexspan, no matter where you start.
Getting Real: Wild Card FAQs, Taboo Truths, and Final Thoughts
Let’s get honest. If you’ve ever wondered whether your sexspan—the period in your life when you feel sexually active and fulfilled—should match your actual lifespan, you’re not alone. The truth? It’s normal for your sexspan to feel shorter than your lifespan, unless you take steps to intervene. There’s no universal “normal” when it comes to sexspan; everyone’s experience is unique, and research shows that shame loses its grip when you turn it into conversation. So, let’s break down some of the most common, and often taboo, questions about sexual health and opening up about sex.
Is It Normal for Your Sexspan to Feel Shorter Than Your Lifespan?
Absolutely. Life throws curveballs—stress, health changes, relationship shifts, and even medications can all impact libido and sexual satisfaction. For example, as mentioned in the transcript (12.25-12.27), culprits for low libido are varied and sometimes surprising. One major factor? Antidepressants. According to the transcript (12.27-12.30), these medications can actually decrease libido, not increase it. If you’ve noticed changes in your sexual desire, you’re not broken or alone.
But here’s the hopeful part: your sexspan isn’t set in stone. With the right sexual health tips and a willingness to talk openly, you can extend your sexspan and redefine what’s possible for you.
How Do You Actually Start These Uncomfortable Conversations?
Opening up about sex can feel daunting. The first step is often the hardest, but it’s also the most important. Try starting with open-ended questions like, “How have you been feeling about our intimacy lately?” or “Is there anything you wish we could talk about more openly?” Sharing personal stories—whether your own or someone else’s—can make the topic less scary and more productive. If you’re not sure what to say, here’s a simple script:
“I’ve been thinking about how important our connection is, and I want us to feel comfortable talking about anything—including sex. Can we check in about how we’re both feeling?”
Remember, it’s always more awkward in your head than out loud. As one wise voice put it: “It’s always more awkward in your head than out loud.” Prove yourself wrong at least once. You might be surprised at how much relief and closeness follow.
Are Medications Ever the Answer?
Sometimes, yes. If you’re struggling with persistent sexual health issues, it’s worth seeing a specialist. Medications can help, but they’re not a one-size-fits-all solution. For example, as the transcript points out, antidepressants can sometimes be the culprit behind a drop in libido. A healthcare provider can help you weigh the pros and cons, adjust dosages, or explore alternatives. Think of it like any other health concern—regular checkups and honest reports are key.
Why ‘One-Size-Fits-All’ Advice Misses the Mark
There’s no magic formula for sexual wellbeing. What works for one person or couple may not work for another. Studies indicate that direct, honest inquiry and openness lead to better outcomes. That’s why it’s so important to approach your own sexspan definition with curiosity, not judgment. Be willing to experiment, adjust, and revisit the conversation as life evolves.
Sidebar: What If We Treated Sexual Health Like Gym Memberships?
Imagine if sexual health got the same attention as physical fitness—annual checkups, goal setting, honest progress reports. Why not? Medical visits for sexual issues should be as routine as other health screenings. Normalizing these conversations is one of the best sexual health tips you can put into practice.
Final Thoughts: Making Sexspan a Lived Experience
In the end, your sexspan is yours to define. Facing taboo topics head-on, asking questions, and sharing stories all help turn sexspan from a buzzword into a real, lived experience. The journey isn’t always smooth, and sometimes the answers raise more questions. But that’s okay. The key is to keep the conversation going—because directness, honesty, and openness are your best allies. And remember, it’s always more awkward in your head than out loud.
TL;DR: Your sexspan is as important as your lifespan—possibly even more, depending who you ask at a dinner party. With the right knowledge (and a willingness to communicate), you can dramatically extend the time you and your partner enjoy meaningful intimacy. Science, honesty, and a few lifestyle tweaks really can make all the difference. Pro tip: never be afraid of a good conversation (even if it gets a bit awkward).
A big shoutout to The Diary Of A CEO for the thought-provoking content! Be sure to check it out here: https://youtu.be/IgW1jepnJp4?si=p0GlpbgdcR5icf0T.