Picture this: You’re sitting at a crowded café, overhearing a group discuss trauma. One person shrugs, calling it a “buzzword.” Another insists it’s a clinical condition reserved for soldiers. And someone quietly, almost defensively, says, “It’s just something from childhood, right?” I’d be lying if I said I hadn’t wondered myself what really counts as trauma – or whether my own rough patches even belong in the conversation. Turns out, even the experts have wrestled with this, but what they’ve discovered might surprise you. Grab your coffee, get comfortable, and let’s reconsider what we mean when we talk about trauma.
1. Trauma Isn’t a Trend: How the Word Got Lost (and Found) Online
If you’ve spent any time online in the last few years, you’ve probably noticed a surge in conversations about trauma. It’s everywhere—on social media, in pop culture, and even in casual chats with friends. But this wasn’t always the case. In fact, the rapid rise in online searches and mentions of “trauma” has surprised even seasoned researchers and mental health professionals (2:55–3:04).
Let’s take a closer look at how trauma, once a taboo subject, has become a central part of today’s mental health trends. This shift isn’t just about language—it’s about how we understand ourselves and each other.
From Taboo to Trending: The Data Behind Trauma Awareness
Research shows there’s been a staggering increase in online searches for “trauma” over the past three decades. While the exact numbers aren’t specified, experts reference a graph that clearly illustrates a huge jump in people using and searching for the word “trauma” (3:04–3:09). This isn’t just a blip. It’s a steady, year-over-year rise that reflects a much broader cultural shift.
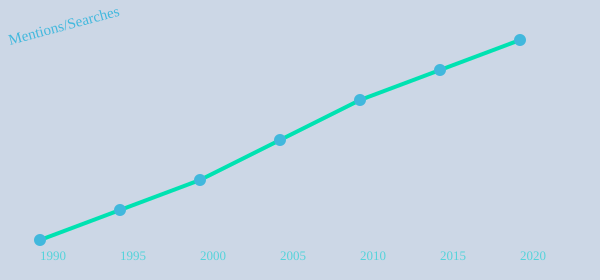
Chart: The rise in online searches and mentions of “trauma” from 1990 to 2020
Why Trauma Awareness Matters—and Why It’s Complicated
Once, trauma was rarely discussed, especially in psychiatric or medical settings. Dr. Bessel van der Kolk, a leading expert in trauma healing, recalls his early days at Harvard, when colleagues questioned why he was even studying trauma. He shares,
“When I first started to study trauma…nobody ever talked about trauma. Now, everything is a trauma.”
(3:21–3:36)
This quote captures the dramatic shift in our collective understanding. Trauma has moved from the shadows into the spotlight, reframing both individual experiences and major historical events. But with this new visibility comes a risk: the term “trauma” can be overused or misunderstood. Some worry that labeling every hardship as trauma might dilute its meaning, fueling trauma misconceptions online.
Connection, Confusion, and the Power of Language
Despite these risks, the mainstreaming of trauma awareness has also brought real benefits. For many, simply having the language to describe their pain is the first step toward trauma healing. As Dr. van der Kolk notes, language helps us organize our internal experiences. Being able to name what happened—whether it’s a personal struggle or a collective crisis—can be oddly validating. It’s a way to connect, not just with others, but with parts of ourselves that may have felt hidden or ignored.
Think about the first time you heard someone casually say, “That was traumatic.” Maybe it felt a little shocking, almost transgressive. But maybe, too, it felt like a relief—a sign that you weren’t alone in your struggles. This is the double-edged sword of today’s mental health trends: more openness, but also more room for confusion.
What’s Driving the Surge?
So, why now? Studies indicate that early life experiences, as well as major historical events, have shaped this surge in trauma awareness. The internet has amplified these conversations, making it easier for people to find information and community. But it’s also created new challenges, as trauma misconceptions online can spread just as quickly.
Ultimately, the evolution of trauma discourse mirrors society’s changing relationship with pain, healing, and mental health. We’re still figuring out what it all means—and that’s okay. The important thing is that we’re talking about it, together.
2. Past Shadows: How Childhood Trauma Shapes Grown-Up Brains and Lives
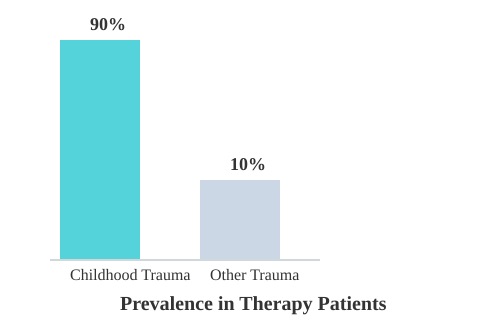
When you think about trauma, you might picture a single, life-altering event—a car accident, a natural disaster, or something equally dramatic. But research shows that the impact of childhood trauma is far more common and complex than many realize. In fact, Dr. Bessel van der Kolk, a leading trauma expert, notes that “about 90% [of patients] have childhood trauma…but yes, change is possible.” (0.42-0.44). That’s not a typo—nine out of ten people seeking trauma-focused therapy are carrying burdens from their early years.
But what exactly counts as trauma? It isn’t always obvious. Sometimes, it’s not about what happened, but what didn’t happen. Years of not being seen, heard, or valued can leave wounds just as deep as any single event. This is where the concept of relational trauma symptoms comes in. You might have grown up in a home where no one yelled or hit, but if you felt invisible, unimportant, or like your feelings didn’t matter, that’s trauma, too (7.29-7.34).
Big T vs. Small t: Why All Trauma Matters
There’s a lot of talk about “Big T” and “small t” trauma. “Big T” is the obvious stuff—abuse, violence, disasters. “Small t” is quieter: chronic neglect, emotional dismissal, or subtle put-downs. Dr. van der Kolk isn’t a fan of this distinction (7.16-7.23). Why? Because the so-called “small t” traumas are very real and can have just as much impact. For example, being told to stop crying or that your feelings don’t matter chips away at your sense of self. Over time, these experiences shape how you see yourself and the world (7.54-8.00).
It’s not just about the event itself, but the context and your subjective experience. If your environment doesn’t acknowledge your existence or emotional needs, that’s a form of trauma. The message you receive—sometimes without a word—is that you don’t matter. And that sticks.
Relational Trauma: The Invisible Wound
Relational trauma is perhaps one of the most under-recognized yet deeply influential forms of childhood adversity. It’s the feeling of being invisible, unvalued, or emotionally abandoned. Maybe your parents were physically present but emotionally unavailable. Or maybe you were blamed for things that weren’t your fault, like being told, “Your dad is a drunk because you’re such a difficult kid” (8.09-8.17). These wounds are subtle, but they cut deep.
Studies indicate that relational trauma symptoms can be just as damaging as more obvious forms of abuse. The effects linger, shaping your self-worth, your relationships, and even your ability to trust others. It’s not uncommon to see adults struggle with intimacy, boundaries, or self-esteem, all rooted in these early experiences.
Your Brain on Childhood Trauma
Here’s where things get even more interesting: childhood trauma impact isn’t just emotional—it’s biological. When you grow up in survival mode, your brain adapts. It rewires itself to keep you safe, but this comes at a cost. You might find yourself always on alert, expecting the worst, or struggling to relax. The world starts to look like a dangerous place, even when you’re safe (7.10-7.16).
This isn’t a sign that your brain is broken. It’s a sign that your brain did exactly what it needed to do to help you survive. But those adaptations can linger long after the danger is gone. The good news? Trauma healing is possible. As Dr. van der Kolk says, change can happen—even after years of living with these patterns.
Anecdote: The Distant Aunt
Think about that distant aunt who never hugged anyone, who always seemed a little cold or withdrawn. There’s a good chance she was carrying her own history of unmet needs and invisible wounds. Sometimes, the behaviors we don’t understand in others are echoes of their own childhood trauma.
“About 90% [of patients] have childhood trauma…but yes, change is possible.” – Bessel van der Kolk
3. Conventional Wisdom vs. Lived Reality: Why Classic Therapies Don’t Always Cut It
When you first hear about PTSD therapy methods, you might picture a therapist’s office, a box of tissues, and a lot of talking. Cognitive Behavioral Therapy (CBT) and exposure therapy are the gold standards—at least according to insurance companies and many treatment guidelines. But if you’ve ever sat through these sessions and wondered why you still feel stuck, you’re not alone. The truth is, classic talk therapies often miss the mark when it comes to the messy, non-verbal reality of trauma (see transcript 4.29-4.40).
Let’s break down why the conventional approach doesn’t always match what people actually experience—and what brain science trauma research is revealing about real healing.
CBT and Exposure Therapy: Revered, But Do They Work for Trauma?
CBT is everywhere. It’s structured, it’s measurable, and it’s easy to standardize. Insurance companies love it because it promises results in a neat, eight-session package. Exposure therapy, another favorite, asks you to face your fears head-on, with the idea that repeated exposure will desensitize you (4.36-4.42).
But here’s the catch: research shows there’s no statistically robust evidence backing the idea that you can “cure” trauma in eight sessions. Real trauma healing is rarely that tidy. People are often taught methods that sound good on paper, but in practice, they don’t always address the core of what trauma does to the mind and body (4.34-4.40).
| Claim | Research Finding |
|---|---|
| Eight-session trauma “cures” | No statistically robust evidence supports these quick-fix methods |
| Trauma recall and brain function | Neuroimaging shows decreased prefrontal (cognitive) activity during trauma recall |
Trauma Is More “Felt” Than “Thought”
Many traditional therapies focus on changing your thoughts. The idea is: if you can just “think differently,” you’ll feel better. But trauma isn’t just a collection of bad thoughts. It’s a deeply felt experience—often beyond words. As Bessel van der Kolk puts it,
“Trauma is a speechless experience…when you’re in your trauma, you’re just one ball of emotion.”
During traumatic flashbacks, neuroimaging studies indicate that the parts of your brain responsible for language and logic—the prefrontal cortex—actually shut down (5.56-6.02). You can’t just reason your way out of terror. Instead, you’re left with confusion, agitation, and a sense of being overwhelmed (6.02-6.14). This is why being told to “just get over it” isn’t just unhelpful—it’s neurologically naive.
The Limits of “Talking Cures”
CBT and similar talk therapies have their place, especially for anxiety or depression. But when it comes to trauma, research shows their effectiveness is limited. The push for quick, standardized solutions often comes from insurance and funding pressures, not from what actually works for people living with PTSD (4.42-4.51).
In fact, many therapists learn these methods in school, but few actually see them work as advertised in real life. The idea that you can “straighten out” someone’s thinking or make them stop having “crazy thoughts” just doesn’t line up with the lived reality of trauma survivors (4.46-5.00).
Brain Science Is Reframing What Heals Trauma
So, what does help? New research in brain science trauma is showing that healing often starts with addressing the non-verbal, bodily experience of trauma. When you’re in the grip of a traumatic memory, you’re not thinking—you’re feeling. Finding language for your experience is important, but it’s not enough on its own (6.27-6.38).
In summary, the gap between conventional wisdom and lived reality is wide. Classic PTSD therapy methods like CBT may help some, but they often miss the non-verbal, emotional core of trauma. Brain science is pushing the field to look beyond quick fixes and embrace approaches that honor the full complexity of healing.
4. The Experiments: Unconventional Paths to Healing Trauma (EMDR, Yoga, Psychedelics)
When you think about healing trauma, talk therapy probably comes to mind first. But what if your brain needs something different—something that doesn’t just rely on words? Over the past few decades, researchers and clinicians like Bessel van der Kolk have pushed the boundaries, exploring unconventional therapies that go far beyond the therapist’s couch. These experiments have changed the way we think about trauma recovery, showing that your brain isn’t broken—it just needs the right tools to heal.
EMDR Effectiveness: Rewiring the Traumatized Brain
Let’s start with EMDR, or Eye Movement Desensitization and Reprocessing. If you haven’t heard of it, you’re not alone. EMDR might sound a bit odd at first—moving your eyes back and forth while recalling painful memories—but research shows it can be transformative. In fact, van der Kolk cites a study where 78% of adults with PTSD were “completely cured” after EMDR sessions (see 1.03-1.05). That’s not just improvement; that’s a life reclaimed.
‘78% of the people we studied who had adult in time were completely cured [with EMDR].’ – Bessel van der Kolk
Why does EMDR work so well? The theory is that it helps your brain process traumatic memories in a new way, reducing their emotional charge. Instead of just talking about what happened, you’re actively helping your mind rewire itself. For many, this is a game-changer, especially when traditional talk therapy hasn’t worked.
Yoga for PTSD: From Fringe to Frontline
Not long ago, the idea of using yoga for PTSD sounded radical. Now, it’s recognized as a powerful tool for reconnecting mind and body after trauma (0.57-1.00). Van der Kolk was one of the first to bring yoga into trauma treatment, and the results were so effective that even skeptics took notice.
Yoga helps you tune into your body—something trauma often disrupts. By focusing on breath and movement, you can start to feel safe in your own skin again. It’s not about flexibility or fancy poses; it’s about regaining control and calm. Personally, I used to scoff at yoga, but after a few classes, I realized my anxiety wasn’t so glued to my muscles anymore. Sometimes, the simplest shifts make the biggest difference.
Psychedelic Therapy Trauma: Breaking Through the Walls
Psychedelic-assisted therapy is another unconventional path that’s gaining attention. It’s controversial, sure, but early research and personal accounts suggest it can lead to deep breakthroughs. For some, psychedelics help confront root pain that’s been locked away for years. Van der Kolk himself has explored these therapies, finding that altered states—when guided safely—can help rewire traumatic imprints in ways talk therapy can’t touch (1.01-1.03).
Of course, this isn’t for everyone, and it’s not a magic bullet. But for those who feel stuck, psychedelic therapy may offer a new route to healing, especially when combined with professional support.
Neurofeedback for Trauma: Watching Your Brain Heal
Imagine if your brain could watch itself in real time and learn to self-correct. That’s the promise of neurofeedback for trauma. Using sensors and computer feedback, neurofeedback helps your brain relearn balance and calm. The results, according to van der Kolk, have been “stunning” for select patients (1.03-1.05).
Neurofeedback doesn’t require you to talk about your trauma at all. Instead, it taps into your brain’s natural plasticity, helping it find new pathways to peace. For some, this is the missing piece they’ve been searching for.
Thinking Outside the Box: Your Own Healing Lab
What if you could design your own unconventional healing lab? Would you invent a quirky tool or blend different therapies? The truth is, healing isn’t one-size-fits-all. The most effective approaches often integrate mind, body, and sometimes even altered states. Research indicates that these innovative therapies can outperform traditional talk therapy for many trauma survivors.
So, if you’ve ever felt stuck or skeptical, remember: your brain isn’t broken. Sometimes, it just needs a new experiment—a fresh path to healing you never expected.
5. The Relational Core: Broken Connections and Repairing What We Missed
When you think about trauma, it’s easy to focus on the event itself—what happened, what was said, or what was lost. But research shows that the real heart of trauma often lies in something much deeper: connection and trauma are tightly linked. It’s not just about what happened to you, but about who was (or wasn’t) there with you when it did (7.54-8.00). This is why so many people struggle with relational trauma symptoms, even when their experiences might seem “small” or trivial to others.
Consider the classic phrases many of us heard growing up: “Stop crying or I’ll give you something to cry about,” or “You’re too much for this family.” These words, and the feelings behind them, send a clear message: you don’t matter (8.00-8.17). Over time, this kind of chronic relational neglect quietly undermines your sense of self-worth. You may have learned to take care of everyone else—your parents, your siblings—while no one made room for your own needs (8.43-8.49). The result? A breakdown of connection with both yourself and others, which is often the deepest wound trauma leaves behind.
It’s interesting to note that most people who seek therapy aren’t coming in because of a single, dramatic event. Instead, they’re struggling with the long shadow of not being seen, heard, or cared for (8.35-8.43). This is what experts call relational trauma. The absence of connection in childhood can lead to lifelong struggles with affection, intimacy, and self-worth. In fact, studies indicate that chronic absence of connection is often more damaging than a single “big” event.
| Type of Trauma | Common Therapy Presentation |
|---|---|
| Relational/Chronic Neglect | Majority of clients report “not being seen” or “not being heard” |
| Single-Event Trauma (e.g., accident, assault) | Less common than chronic neglect as a primary complaint |
Let’s look at how this plays out in real life. After a natural disaster, you might see neighbors who never spoke before suddenly banding together, helping each other, and forming new bonds. I once spent a summer helping out after a local flood and saw this firsthand—people who’d lived side by side for years became rescuers overnight. That sense of connection, even in crisis, can be incredibly healing. But when neglect is chronic and quiet, there’s no dramatic event to unite people. Instead, the pain lingers, unspoken and unresolved.
So, how do you begin repairing what was missed? Trauma healing isn’t just about revisiting the past or analyzing what went wrong. It’s about building new connections—starting with yourself. Self-compassion is a crucial first step. Learning to be gentle with yourself, to recognize your own needs, and to believe that you matter can slowly rebuild the foundation that was missing. Safe relationships are equally important. Finding people who truly see and hear you—who accept you as you are—can transform your sense of self and your ability to trust.
Vulnerability is another essential ingredient. It’s not easy to open up when you’ve been hurt, but allowing yourself to be seen, even in small ways, is a powerful act of healing. As Bessel van der Kolk puts it:
“The issue is not the event itself. You and I may have the same events happening, but for me, it’s a very big deal…”
Ultimately, the most important question in trauma healing may be: Who truly sees and hears you? When you can answer that, you’re already on the path to repairing the relational core that trauma once fractured.
6. The Scientist and the Patient: How Personal History Shapes Professional Passion
When you think about childhood trauma impact, it’s easy to imagine it as something that happens to “other people.” But even the world’s leading trauma experts are not immune. Take Bessel van der Kolk, for example. His story begins in the most turbulent of times—born in 1943, right in the heart of Nazi-occupied Netherlands (11.18-11.22). Rockets thundered overhead, hunger was everywhere, and families like his lived in constant fear and deprivation. It’s no wonder that his life’s work would revolve around understanding trauma and, ultimately, trauma healing.
Van der Kolk’s earliest memories aren’t just his own—they’re shaped by the world he was born into. As he puts it,
“When you’re born has a huge inflict on who you become.”
(11.22-11.25). His father was detained by the Germans, narrowly escaping a worse fate, while his mother was left to raise five children in hiding, right next to the launch sites of Nazi rockets (11.29-11.46). Half of those rockets, he recalls, landed in their own backyard.
What’s striking is that van der Kolk doesn’t remember these events consciously. He describes it as a preconscious imprint—the kind of deep, bodily memory that shapes you even if you can’t put it into words (11.54-12.11). He likens his childhood to what children in Ukraine or Gaza might experience today: a world where hunger, illness, and loss are everyday realities. In fact, he was a sickly child, and half his generation died from starvation (12.02-12.10). This is the very definition of intergenerational trauma—where the pain and fear of one generation ripple into the next, even if no one talks about it.
But the story doesn’t end with war and hunger. Van der Kolk’s mother, too, was deeply affected by her own past. She had lived through the 1919 pandemic, which left her father with parkinsonism and changed her family forever (12.42-12.53). The result? She became, in van der Kolk’s words, a “frozen person”—emotionally distant, unable to offer the warmth and affection a child needs (12.56-13.10). If you grew up with a parent who struggled to show love, you might recognize this. It shapes your view of the world, making closeness and vulnerability feel foreign or even unsafe.
Research shows that these early experiences—especially those involving attachment and care—can have a profound childhood trauma impact. If your parent is emotionally unavailable, it can take years of work to learn about affection, intimacy, and trust (13.10-13.33). For van der Kolk, this personal wound became a professional curiosity. He wanted to understand why some people struggle to connect, and why trauma seems to echo down family lines, even when no one speaks of it.
This is where the line between scientist and patient blurs. Sometimes, the drive to help others heal comes from a need to make sense of your own story. Van der Kolk recognized the echoes of trauma in his patients long before most psychiatrists were willing to acknowledge its power. His expertise didn’t just come from textbooks—it grew from lived experience, from a need to heal something personal. Studies indicate that personal history often steers professional specialization, especially in caring or investigative fields. In other words, the best healers are often those who have had to heal themselves.
There’s a quirky thought experiment that often comes up in trauma work: If you could time-travel and observe your parents as children, would you? Would you really want to know what shaped them, what wounds they carried? Sometimes, understanding the roots of intergenerational trauma means facing uncomfortable truths about our own families. But it’s also the first step toward real trauma healing—breaking the cycle, so the pain doesn’t keep passing down the line.
Van der Kolk’s story is a powerful reminder that trauma isn’t just something that happens to us—it’s something we inherit, carry, and, with understanding and compassion, can begin to heal. His journey shows that the path to expertise often starts with a personal question: Why did my life turn out this way? And how can I help others find a different answer?
7. Myths, Mistakes, and Moving Forward: Rethinking What Trauma Really Means
If you spend any time online, you’ve probably noticed how the language of trauma has seeped into everyday conversation. It’s almost a cultural joke now—someone says they’re “triggered” by a bad day at work, or claims to be “traumatized” by a minor inconvenience (6.48-6.51). But what actually counts as trauma? Is it only the “big” stuff, or can smaller, less obvious experiences leave a mark too? These questions are at the heart of many trauma misconceptions online, and they matter more than you might think.
Let’s start by clearing up a common mistake: not every setback or stressful moment is trauma. At the same time, not all trauma is obvious or dramatic. Trauma is, at its core, an overwhelming experience—one that leaves you feeling helpless, with no idea how to cope (6.58-7.13). It’s not about the event itself, but about how it lands in your mind and body. As trauma expert Bessel van der Kolk puts it,
“The issue is not the event itself…the issue is your perception.”
This is where things get complicated. Two people can go through the exact same event and walk away with completely different reactions. For one, it might be a blip on the radar. For the other, it could trigger deep pain, memories, or fear (9.07-9.59). There’s no universal trauma scale—no checklist that says, “This counts, but that doesn’t.” Research shows that trauma healing is deeply personal, and that a nuanced, individualized approach is key to honest recovery.
You might have heard terms like “big T” and “small t” trauma. Some experts aren’t fans of these labels, because they can oversimplify what is a very personal experience (7.16-7.23). Sure, a natural disaster or violent event is traumatic for many. But being ignored, dismissed, or made to feel invisible can also be deeply wounding—especially if your environment doesn’t acknowledge your existence (7.29-7.34). The context, your history, and your perception all play a role.
Pop culture’s casual use of “triggered” and “traumatized” can sometimes trivialize real suffering. It’s easy to roll your eyes at the overuse, but there’s another side to it. This language, even when used lightly, has helped destigmatize mental health struggles. More people feel comfortable talking about their pain, seeking help, and starting their own personal trauma journey. That’s a positive shift, even if it means we sometimes blur the lines between discomfort and true trauma.
Still, overusing the word “trauma” can muddy the waters. When everything is trauma, nothing is. It’s important to respect the difference between a tough day and a life-altering wound. But it’s just as important to remember that your pain is valid, even if it doesn’t fit someone else’s definition. Healing isn’t about fitting into a box—it’s about discovering what you need to move forward.
So, what does moving forward look like? It means looking past the label and asking yourself: What do you need to heal? Not what the internet says, not what your friends or family think, but what feels true for you. If there were a blood test for trauma, would you want to take it? And if you did, what would you do with the result? Would it change how you see yourself, or how you approach your healing?
The truth is, there’s no test, no universal answer. Trauma is contextual and subjective, shaped by your past, your environment, and your perception. The most honest path to healing is the one that honors your experience—messy, nuanced, and uniquely yours. As you continue your personal trauma journey, remember: your brain isn’t broken. With understanding and the right support, healing really does happen, often in surprising ways.
TL;DR: Trauma is more nuanced than we realize—shaped by our brains, our relationships, and our histories. Healing is possible with approaches that go beyond talk therapy. Your story, and your pain, matter more than you know.
Hats off to The Diary Of A CEO for their thought-provoking content! Take a look here: https://youtu.be/Qx5J5nwDBTo?si=CZJeNKguUUbFhiIy.